Cardiomyopathy
What is cardiomyopathy?
Cardiomyopathy (pronounced card-ee-oh-my-OP-ah-thee) is a disease of the heart’s muscular wall, called the myocardium. It can cause changes that make the heart muscle weak, stiff or both.
When the heart muscle is not strong enough to pump blood out the body or it cannot relax enough to let blood into the ventricles, this can lead to congestive heart failure. Children with cardiomyopathy are also at risk for an abnormal heart rhythm (arrhythmia).
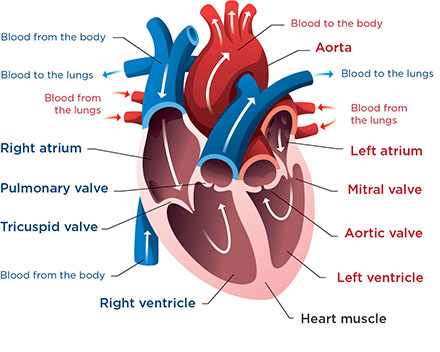
This is a normal heart. It sends oxygen-rich blood to the body through the aorta and oxygen-poor blood to the lungs through the pulmonary artery.
There are 3 main kinds of cardiomyopathy:
-
Dilated cardiomyopathy
In this kind, the heart muscle is weakened, and the heart becomes enlarged and stretched. As the heart works harder to try keeping up with the body’s needs, it can get bigger and become weaker over time. This is the most common kind of cardiomyopathy in children.
There are several causes:
- Certain infections (usually viral) can irritate the heart muscle (a condition called myocarditis) and weaken it. In many cases, the infection can be treated and the heart muscle can recover, but sometimes the damage is permanent.
- Sometimes children born with other heart conditions develop dilated cardiomyopathy. This can happen because of the heart condition or surgeries they have had or because the heart muscle gets tired and weak over time.
- Some medicines can injure the heart muscle. One example is chemotherapy for cancer.
- Some kinds of arrhythmias – if they go on for a long time – can cause the heart muscle to become weak.
- Some forms of dilated cardiomyopathy are genetic, meaning the disease can be passed down from parents to children in their genes. Genetic cardiomyopathies often run in families.
Sometimes, doctors cannot find a cause. They call this idiopathic dilated cardiomyopathy.
-
Hypertrophic cardiomyopathy
In this kind, the heart muscle is too thick. This can cause problems in how the heart relaxes and fills with blood, how it pumps blood out to the body or both. Hypertrophic cardiomyopathy can also cause abnormal heart rhythms.
Usually, this kind of cardiomyopathy is caused by a problem with genes that affect how the heart muscle develops. Some babies born with this condition show signs at birth. But in many people, it is not diagnosed until later in life. Hypertrophic cardiomyopathy can also happen after birth because of another health problem, such as a hormone problem that causes excess growth (acromegaly).
-
Restrictive cardiomyopathy
In this kind, the heart muscle becomes very stiff, making it harder for the ventricles to fill with blood between heartbeats. This is the least common kind of cardiomyopathy in children. It is sometimes linked with a gene problem, but often doctors cannot find a cause.
The condition can happen in babies whose heart lining is thicker than normal.
It can also develop in children if another condition or treatment causes scar tissue to build up in their heart muscle. One example would be radiation therapy for cancer.
Cardiomyopathy Care at Seattle Children's
Symptoms of Cardiomyopathy
Babies with cardiomyopathy may have these symptoms:
- Working hard to breathe
- Having poor appetite or trouble feeding
- Failure to thrive
In older children, the first symptoms are often shortness of breath when active and feeling more tired than normal. Some children develop arrhythmia or palpitations. Other symptoms can include fainting and chest pain.
If your child has an infection that causes cardiomyopathy, you may first notice symptoms of the infection. These can include fever, chills or feeling weak or achy.
As the heart gets weaker, your child may develop other symptoms of congestive heart failure, such as trouble breathing, poor appetite, nausea, vomiting or edema.
Diagnosing Cardiomyopathy
To diagnose this condition, your child’s doctor will examine your child and use a stethoscope to listen to their heart.
The doctor will ask for details about any symptoms your child has, their health history and your family health history.
To get more information about how their heart looks and works, your child will need some tests. Your child’s doctor may use echocardiography and an electrocardiogram to aid in the diagnosis. Sometimes the doctor needs more information and will order chest X-rays or an MRI (magnetic resonance imaging) of the heart.
Many children need lab tests (blood draws) to help find a cause for the cardiomyopathy and to see how their other organs are handling heart failure.
Sometimes children need cardiac catheterization.
Treating Cardiomyopathy
Doctors usually treat cardiomyopathy with medicines. Some children may need a pacemaker or defibrillator. Some children’s hearts may be so weak that they require a machine (ventricular assist device) to help do the work of the heart. This is called mechanical circulatory support. In rare cases, a child with this condition needs a heart transplant.
If doctors can find an underlying cause, such as an infection or hormone problem, they will treat this, too.
-
Medicine
To help the heart pump better, doctors use medicines like these:
- Angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs), which reduce the workload on the heart and can slow the worsening of cardiomyopathy.
- Entresto, a newer medicine that combines an ARB (valsartan) with another medicine called sacubitril. These work together to better reduce the workload of the heart and slow the worsening of cardiomyopathy.
- Beta-blockers, which reduce the workload on the heart by lowering the blood pressure and slowing the heart rate.
- Digoxin, which makes the heart beat slower and with more force.
- Diuretics, which help the kidneys rid the body of extra water via the urine. This lowers the amount of fluid in the lungs and other tissues and may improve heart failure symptoms.
- Anticoagulants, or anticlotting medicines, which help prevent or dissolve clots that might form in the heart or blood vessels. When the heart is enlarged and weak, blood flow is slower, which may lead to clots forming.
- Medicines that correct the heart rate or make an irregular heartbeat normal if your child needs treatment for arrhythmia.
-
Pacemaker
A pacemaker is a small device that doctors implant in your child’s chest. A wire attaches the pacemaker to an electrode. The electrode is placed in the heart wall. Small electrical impulses travel from a special battery through the wire to the heart, telling the heart when to beat.
-
Defibrillator
A defibrillator is similar to a pacemaker.\
It monitors your child’s heart all the time for life-threatening rhythm problems. When it detects a problem, it sends an electrical shock to the heart to bring it back to a normal rhythm.
-
Ventricular assist device (VAD)
Sometimes, a child’s heart can become so weak that it needs more help than medicines can provide. In these cases, cardiac surgeons can connect the child’s heart to a mechanical pump that does the work of the heart. This kind of pump is called a VAD, and it can be placed inside or outside the body. VADs can support either the left or right ventricle or both. A VAD can be used for patients waiting for a heart transplant or for patients whose heart muscle needs time to rest and recover from an injury or infection.
AJ’s Story
When a virus attacked AJ’s heart, his team at Seattle Children’s recommended a ventricular assist device (VAD). The CentriMag pump allowed his heart to rest, heal and recover.
-
Transplant
The heart transplant team at Seattle Children’s performs many transplants each year for children with cardiomyopathy or other heart problems that cannot be controlled using other treatments. Read more about our heart transplant program.
Cardiomyopathy at Seattle Children’s
 For more than a decade, U.S. News & World Report has consistently ranked our Heart Center among the top pediatric cardiology and heart surgery programs in the country, which means your child will be cared for by the very best.
For more than a decade, U.S. News & World Report has consistently ranked our Heart Center among the top pediatric cardiology and heart surgery programs in the country, which means your child will be cared for by the very best.
 We Are a Cardiomyopathy Center of Care
We Are a Cardiomyopathy Center of Care
Seattle Children’s Heart Center has been named a Cardiomyopathy Center of Care by the Children’s Cardiomyopathy Foundation (CCF), a national nonprofit committed to improving health outcomes and quality of life for children with cardiomyopathy. Seattle Children’s received this recognition for consistently providing high-quality cardiac care and specialized disease management for children with all forms of cardiomyopathy.
Centers are recognized based on meeting CCF’s criteria of managing a high volume of cardiomyopathy patients; offering a variety of pediatric services; specializing in the treatment and management of cardiomyopathy in children; and affiliation with an academic research institution.
-
The experts you need are here
- Our team of 40+ pediatric cardiologists diagnoses and treats cardiomyopathy in children of all ages, from infants to young adults.
- A dedicated group of these doctors specializes in caring for children with cardiomyopathy and heart failure. They work closely with other Heart Center specialists – like our pediatric cardiac surgeons, cardiac catheterization team, electrophysiology team and cardiac nurses, nutritionists and pharmacists – to provide the highest level of care.
- Our 4 cardiac surgeons perform more than 500 procedures yearly. They have deep experience operating on babies, children and teens who need surgery, like placement of a pacemaker, defibrillator or ventricular assist device or a heart transplant.
- We also have a pediatric cardiac anesthesia team and a Cardiac Intensive Care Unit ready to care for children who undergo heart surgery.
- If your child has more than 1 condition, we make sure they get all the care they need. We involve doctors from other Seattle Children’s teams to meet your child’s needs, such as doctors who specialize in the kidneys, lungs or gastrointestinal system or the health of newborns. Heart Center doctors work closely with oncologists if cancer treatment affects your child’s heart.
 “I can’t imagine getting any better care than what Adrian had at Seattle Children’s. Each team was always extremely helpful and informative. We knew exactly what was going on from an hour-to-hour, day-to-day basis.”
“I can’t imagine getting any better care than what Adrian had at Seattle Children’s. Each team was always extremely helpful and informative. We knew exactly what was going on from an hour-to-hour, day-to-day basis.” -
Among the nation’s top programs
- Our Heart Failure Program is the only subspecialty of its kind in the Northwest.
- Our surgical outcomes are among the best in the nation year after year.
- Seattle Children’s has been named a Cardiomyopathy Center of Care by the Children’s Cardiomyopathy Foundation. The foundation is a national nonprofit committed to improving the health outcomes and quality of life for children with this condition.
-
Care from birth through young adulthood
- We match your child’s care to their symptoms and needs. Some children need only medicines for cardiomyopathy. Others need an implanted device to help their heart beat or to take over some of the heart’s work. In the most severe cases, a child may need a heart transplant. Your child’s treatment plan is custom-made for them.
- With regular visits and careful monitoring, we check how your child is doing over time. As their needs change, we adjust their care to get the best results. We always take into account their age, growth and development.
- At Seattle Children’s, we have the expertise to take care of children of all ages, from newborns to young adults.
-
Support for your whole family
- We are committed to your child’s overall health and well-being and to helping your child live a full and active life.
- Whatever types of care your child needs, we will help your family through this experience. We will discuss your child’s condition and treatment options in ways you understand and involve you in every decision.
- Our child life specialists know how to help children understand their illnesses and treatments in ways that make sense for their age.
- Seattle Children’s has many resources, from financial to spiritual, to support your child and your family and make the journey as smooth as possible.
- Many children and families travel to Seattle Children’s for heart surgery or other care. We help you coordinate travel and housing so you can stay focused on your child.
-
Research to improve care
- Doctors and scientists at Seattle Children’s are working to advance treatment for cardiomyopathy and enhance the quality of life for children living with this condition.
- We take part in multicenter clinical trials to study medicines for children with cardiomyopathy and heart failure and ways to improve outcomes for children who have ventricular assist devices or need a heart transplant.
Research and Clinical Trials
Seattle Children’s has been involved in multicenter clinical trials to study medicines for children with cardiomyopathy and heart failure, including a recent study testing a new medicine, Entresto (sacubitril/valsartan).
We belong to ACTION – Advanced Cardiac Therapies Improving Outcomes Network. This national group works to improve care for children with ventricular assist devices.
Our researchers are also focused on improving outcomes for children who need a heart transplant. We are part of multicenter trials comparing transplant approaches and are studying medicines used long term to prevent transplant rejection.
Contact Us
Contact the Heart Center at 206-987-2515 for an appointment, second opinion or more information.
Providers, see how to refer a patient.
Related Links
Conditions
Treatments
Video
Paying for Care
Learn about paying for care at Seattle Children’s, including insurance coverage, billing and financial assistance.

