Arrhythmia
What is arrhythmia?
Arrhythmia (pronounced a-RITH-me-ah) is an abnormal heart rhythm. Typically, this means a child’s heart is beating too fast or too slow for the activity they are doing.
There are many kinds of arrhythmia that affect the heart in different ways. In some children, an abnormal heartbeat may have serious effects. But in many cases the arrhythmia is harmless, even though the symptoms might be a bother.
Children with signs and symptoms of arrhythmia should be checked by a heart doctor (cardiologist).
-
What causes arrhythmia?
Arrhythmias are caused by a problem with the electrical system in the heart.
Some arrhythmias are present at birth (congenital), and others start after an event such as an infection of the heart or heart surgery.
For example, supraventricular tachycardia (SVT) is the most common cause of a fast heartbeat. It is usually not life threatening. In contrast, long QT syndrome is a genetic condition linked with life-threatening arrhythmias that may be triggered by exercise or by being startled or frightened.
In other cases, such as after heart surgery, the heart’s normal electrical system may become scarred and not function normally. This may cause very rapid heartbeats or a heartbeat that is too slow for the child’s level of activity.
-
How a normal heartbeat happens
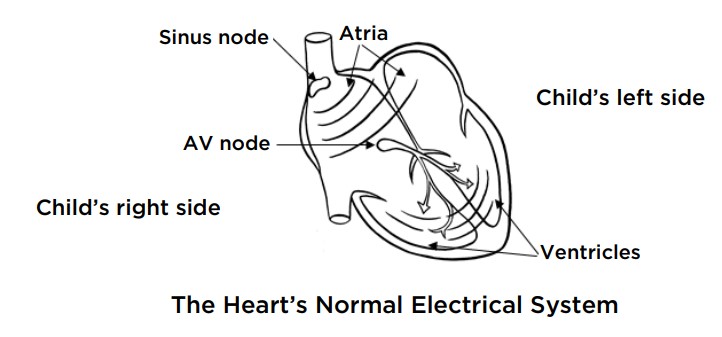
- The heart has 4 chambers that work like a pump. The atria are the 2 top chambers. They receive blood from the lungs and the rest of the body. The ventricles are the 2 bottom chambers. They pump blood out to the lungs and the rest of the body. All 4 chambers need to work in time with each other for the heart to pump well.
- The sinus node, at the top of the right atrium, is the “pacemaker” of the heart. It works to control the heart rate. It makes the heart beat slower during times of rest or sleep and beat faster with exercise or when you are scared or excited.
- Each heartbeat begins with an electrical wave (signal) that passes from the sinus node through the upper chambers of the heart. This signal travels much like the ripples made in water when you throw in a pebble. It makes the atria squeeze, or beat.
- Next, the signal moves into the junction between the upper and the lower chambers. This spot is known as the atrioventricular node (AV node). The AV node delays the signal slightly and then passes it on to the ventricles, making them beat.
- After the ventricles beat, the heartbeat cycle is complete. There should be no way for the electrical signal to travel backwards up to the atria. Rather, the next heartbeat should start in the sinus node and follow the same path.
Heart Center at Seattle Children's
What are the symptoms of arrhythmia?
Arrhythmia can cause these problems with your child’s heartbeat:
- Heart beats too slowly (bradycardia, pronounced brad-ih-CARD-ee-ah).
- Heart beats too quickly (tachycardia, pronounced tack-ih-CARD-ee-ah).
- Heartbeat is irregular — the speed and pattern change.
You and your child might not notice any problems with their heartbeat. Sometimes families have no idea their child has an arrhythmia until it is found during a routine exam.
Because the heartbeat affects blood flow, some arrhythmias can cause these signs and symptoms:
- A sense of an unusual heartbeat (palpitations)
- Feeling faint, weak, lightheaded or dizzy
- Being short of breath
- Tiring easily
- Having chest pain
- Sweating
- Ashen skin or paler skin than is usual for your child
How is arrhythmia diagnosed?
To diagnose this condition, your child’s doctor will examine your child, check their heartbeat and use a stethoscope to listen to their heart. The doctor will ask for details about any symptoms your child has, their health history and your family health history.
Some kinds of arrhythmia happen only once in a while. When they are not happening, they can be difficult to diagnose.
To reach a diagnosis, your child may need some or all of these tests:
-
Electrocardiogram (ECG)
To learn about the electrical signals in your child’s heart, the doctor will use an electrocardiogram. If an abnormal heartbeat does not happen during this test, we may ask your child to wear a monitor at home.
Learn more about what to expect with an ECG.
-
Holter monitor or event monitor
Wearing a monitor at home may help doctors diagnose an abnormal heart rhythm that did not happen during your child’s ECG. It can also help us learn more about an abnormal rhythm that the ECG did detect.
The type of monitor depends on your child’s symptoms and age.
- For daily symptoms, children typically use a device called a Holter monitor. It can record the heart’s activity for 24 hours.
- For less frequent symptoms, children may use an event monitor. You or your child can start it when your child feels a problem with their heart rhythm.
Learn about what to expect with a Holter monitor or event monitor.
-
Electrophysiology (EP) studies
Our doctors use electrophysiology studies to find the cause of an arrhythmia and, in many cases, cure it.
During an EP study, a heart doctor (cardiologist) guides small plastic tubes (catheters) to the heart through the blood vessels of the leg to read the heart’s electrical signals. An EP study is most often used to find the cause of an abnormal heart rhythm. It is sometimes used to tell if a child needs a pacemaker or defibrillator.
If the cause of an arrhythmia is found during an EP study, the doctor may use a form of transcatheter ablation to correct the problem.
-
Other tests
Other common tests for arrhythmia include:
- Echocardiogram
- Exercise testing
- Chest X-ray or MRI (magnetic resonance imaging) of the heart
- Blood tests
How is arrhythmia treated?
Your child may not need any treatment for arrhythmia. Often, an abnormal heartbeat does not cause any problems.
The need for treatment depends on many factors, including:
- The kind of arrhythmia
- Your child’s age
- How often the arrhythmia happens and how long it lasts
- Whether your child has symptoms
If your child does need treatment, there may be several options based on the kind of arrhythmia and how serious it is.
-
Observation
This means checking your child’s condition over time without treatment. The doctor looks for signs that the arrhythmia might be getting worse or could start to affect your child’s health.
-
Medicines
These may be used to correct your child’s heart rate or make an irregular heartbeat steady. The option to use medicine depends on the reason for your child’s arrhythmia and whether doctors can cure it with a procedure like transcatheter ablation.
-
Transcatheter ablation
Just a few decades ago, many children needed heart surgery for arrhythmias that were difficult to treat. Now, doctors can correct many of these arrhythmias with transcatheter ablations.
- During a transcatheter ablation, the doctor guides a small tube (catheter) through the blood vessels of the leg up to the abnormal area in the heart.
- Then, the doctor destroys the small piece of tissue that is causing the problem. They either burn (cauterize) the tissue (radiofrequency ablation) or freeze the tissue (cryoablation).
- The method used depends on the location of the tissue within the heart and how close it is to the heart’s normal electrical system.
-
Pacemaker and defibrillator implantation
Children with certain heart conditions may need a pacemaker or defibrillator to restore and control the rhythm of their heart. Pacemakers are small electronic devices that help control the speed and pattern of the heartbeat. They check the heart rhythm and send an electrical impulse to the heart when it beats too slowly or in an irregular way.
A defibrillator is similar to a pacemaker. It checks the heart at all times for life-threatening rhythm problems such as ventricular tachycardia or ventricular fibrillation. These arrhythmias can lead to sudden cardiac arrest (the heart stops beating) and death if not treated. When the defibrillator finds 1 of these rhythm problems, it sends an electrical shock to the heart to bring it back to a normal rhythm.
Why choose Seattle Children’s for arrhythmia treatment?
Seattle Children’s has a special Arrhythmia Program that provides comprehensive evaluation and treatment for children with heart rhythm problems.
-
The experts you need are here
- The Heart Center team includes more than 40 pediatric cardiologists who diagnose and treat every kind of heart problem. We have treated many children with heart rhythm problems — from simple to complex.
- Experienced doctors in our Arrythmia Program offer the full range of treatment options, like medicines, transcatheter ablation and pacemaker and defibrillator
- Seattle Children’s was the first hospital in the Pacific Northwest to establish a program to offer pediatric electrophysiology and pacing services. At our Electrophysiology Clinic, we diagnose new patients, assess patients with known heart conditions and check patients who have pacemakers and defibrillators.
- Our program has 4 pediatric electrophysiologists, which is uncommon among children’s hospitals. There are only about 200 of these specialists in the United States.
- We perform specialized procedures called electrophysiology studies and transcatheter ablation in our state-of-the-art cardiac catheterization labs. We use the most current technology, such as cryoablation, a method that makes procedures even safer for our patients.
- We also have a pediatric cardiac anesthesia team to make sure that your child is comfortable and safe during arrhythmia procedures.
-
Care from birth through young adulthood
- Seattle Children’s cardiologists see babies, children and teens with arrhythmias. We have experience diagnosing and treating this condition in kids of all ages.
- Your child’s treatment plan is custom-made. Doctors in the Arrythmia Program and Electrophysiology Clinic will review your child’s symptoms, health history and test results to create a plan of care just for your child. We closely check your child’s needs to make sure they get the care that is right for them as they grow.
- If your child was born with a heart condition, we have a special Adult Congenital Heart Disease Program to meet their long-term healthcare needs. This program, shared with the University of Washington, transitions your child to adult care when they are ready.
-
Support for your whole family
- Whatever types of care your child needs, we will help your family through this experience. We will discuss your child’s condition and treatment options in ways you understand and involve you in every decision.
- Our Child Life specialists know how to help children understand their illnesses and treatments in ways that make sense for their age.
- Seattle Children’s has many resources, from financial to spiritual, to support your child and your family and make the journey as smooth as possible.
- Many children and families travel to Seattle Children’s for care. We help you coordinate travel and housing so you can stay focused on your child.
- Read more about the supportive care we offer.
-
Research to improve care and quality of life
- Seattle Children’s doctors are studying technologies to refine arrhythmia care and get the best possible outcomes for children. These include using virtual reality to see a child’s heart in 3 dimensions and robotic arms to move treatment tools with great precision.
- Dr. Stephen Seslar is an international leader in developing a patient registry so doctors everywhere can pool data about arrhythmia care. The registry allows doctors to learn more about the best ways to care for children who have an electrophysiology study or transcatheter ablation.
- Research by Dr. Jack Salerno has helped doctors tell which children with arrhythmia are at risk for sudden cardiac arrest (the heart suddenly stops beating) and how they can safely take part in sports. This work has allowed more children to return to activities that matter to them.
Who’s on the team?
Our Arrhythmia Program includes pediatric cardiologists, cardiac nurses, cardiac nurse practitioners, pediatric anesthesiologists and pediatric cardiac surgeons to ensure that your child gets the best care possible.
Cardiologists
Research and Clinical Trials
Doctors at Seattle Children’s study ways to improve care for children with conditions that can cause arrhythmia. This includes research by Dr. Stephen Seslar using virtual reality technology to give doctors a 3-dimensional view of a child’s heart during procedures, rather than only 2-dimensional images on a flat screen. Seslar also studies the use of robotic arms to hold and precisely move the tools used in treatment. Research like this is designed to get better results for patients.
Seslar also led a project known as MAP-IT. The project created a registry of children, as well as adults, with congenital heart disease who had an electrophysiology study or transcatheter ablation. The purpose is to collect details that can help doctors everywhere improve outcomes and reduce complications. MAP-IT stands for Multicenter Pediatric and Adult Congenital EP Quality Initiative. It began as a project of the Pediatric and Congenital Electrophysiology Society and is now part of the American College of Cardiology’s IMPACT (Improving Pediatric and Adult Congenital Treatment) registry.
For children with some kinds of arrhythmia, there is a risk the heart could suddenly stop beating (sudden cardiac arrest). This is rare but serious. Exercise or other strenuous activity may increase the risk. Dr. Jack Salerno has researched ways to screen athletes for this risk, provide follow-up care they may need and return them safely to sports whenever possible. He co-authored the American Academy of Pediatrics 2021 policy statement on sudden cardiac arrest and sudden cardiac death in children.
Contact Us
Contact the Heart Center at 206-987-2515 for an appointment at the Arrhythmia Program, a second opinion or more information.
Providers, see how to refer a patient.
Related Links
- Cardiac Catheterization Procedures
- Cardiac Catheterization: What to Expect
- Event Monitor: What to Expect
- Heart Center
- Holter Monitor: What to Expect
- Pacemaker and Defibrillator Implantation: What to Expect
Paying for Care
Learn about paying for care at Seattle Children’s, including insurance coverage, billing and financial assistance.






