Advancing the Future of Pediatric Neuroscience Research
Published

The scientists and physician-researchers in Seattle Children’s Research Institute’s Norcliffe Foundation Center for Integrative Brain Research play a pivotal role in the rapid evolution of neuroscience research to advance Children’s mission to provide hope, care and cures to kids everywhere.
Here are some of the latest research findings and advancements from Seattle Children’s neuroscientists and neurologists, and a look at what’s to come:
Protecting Kids’ Brains from Neurotoxicity
 Juliane Gust, MD, PhD is a pioneer in the field of CAR T cell neurotoxicity, having been among the first to publish foundational research on the neurocognitive side effects of these emerging immunotherapies in both adult and pediatric patients. Driven by a passion for ensuring cancer survival without cognitive compromise, her work and lab, focus on the complex intersection of neurology, oncology and immunology. Dr. Gust’s research aims to understand how inflammation and cancer affect the developing brain, particularly the interaction between the immune system and the brain's vasculature, with the ultimate goal of building safer, more efficient CAR T cell treatments and improving long-term neurocognitive outcomes and quality of life for pediatric cancer patients.
Juliane Gust, MD, PhD is a pioneer in the field of CAR T cell neurotoxicity, having been among the first to publish foundational research on the neurocognitive side effects of these emerging immunotherapies in both adult and pediatric patients. Driven by a passion for ensuring cancer survival without cognitive compromise, her work and lab, focus on the complex intersection of neurology, oncology and immunology. Dr. Gust’s research aims to understand how inflammation and cancer affect the developing brain, particularly the interaction between the immune system and the brain's vasculature, with the ultimate goal of building safer, more efficient CAR T cell treatments and improving long-term neurocognitive outcomes and quality of life for pediatric cancer patients.
First-Ever Treatment Progress in Hypothalamic Obesity
 Testing the medication setmelanotide in a first-of-its-kind multicenter clinical trial, Dr. Christian Roth and colleagues found it significantly reduced weight and hunger in patients with hypothalamic obesity, long considered resistant to treatment. There are currently no FDA-approved treatments specifically for hypothalamic obesity, so the findings hold promise for the development of effective and well tolerated treatments for the management of this complex condition.
Testing the medication setmelanotide in a first-of-its-kind multicenter clinical trial, Dr. Christian Roth and colleagues found it significantly reduced weight and hunger in patients with hypothalamic obesity, long considered resistant to treatment. There are currently no FDA-approved treatments specifically for hypothalamic obesity, so the findings hold promise for the development of effective and well tolerated treatments for the management of this complex condition.
Identifying Genetic Variants in Sudden Unexpected Infant Death
 Dr. Nino Ramirez and collaborators, including researchers in Microsoft’s AI for Good Lab, are among the first to use whole genome sequencing to gain insights into potential genetic factors contributing to infants’ vulnerability to sudden unexpected infant death (SUID). The findings significantly expand the list of potential gene variants associated with SUID and include genes related to heart disease, metabolic disorders and neurological conditions, particularly epilepsy. The researchers predict that early detection of a genetic vulnerability can potentially prevent the deaths of infants, as well as adults: Every day, more than 1,000 people die of sudden cardiac death and from epilepsy.
Dr. Nino Ramirez and collaborators, including researchers in Microsoft’s AI for Good Lab, are among the first to use whole genome sequencing to gain insights into potential genetic factors contributing to infants’ vulnerability to sudden unexpected infant death (SUID). The findings significantly expand the list of potential gene variants associated with SUID and include genes related to heart disease, metabolic disorders and neurological conditions, particularly epilepsy. The researchers predict that early detection of a genetic vulnerability can potentially prevent the deaths of infants, as well as adults: Every day, more than 1,000 people die of sudden cardiac death and from epilepsy.
Leading Genetic Diagnostic Research for Epilepsy
 Edward “Rusty” Novotny, MD, who researches refractory epilepsy genetics and directs Seattle Children’s Epilepsy Program (the only level 4 epilepsy center in the Pacific Northwest dedicated exclusively to pediatrics), received the 2025 Arthur A. Ward, Jr. Achievement in Epilepsy Award from the Epilepsy Foundation Washington to honor his leadership and accomplishments over decades. He and his team conduct genetic testing to help diagnose epilepsy syndromes and pinpoint the cause of seizures. This testing also helps families understand the chances of a genetic disorder in subsequent pregnancies. Dr. Novotny’s clinical efforts are closely integrated with ongoing bench research aimed at understanding the cellular mechanisms underlying intractable epilepsy, which involve somatic mutations in the mTOR pathway.
Edward “Rusty” Novotny, MD, who researches refractory epilepsy genetics and directs Seattle Children’s Epilepsy Program (the only level 4 epilepsy center in the Pacific Northwest dedicated exclusively to pediatrics), received the 2025 Arthur A. Ward, Jr. Achievement in Epilepsy Award from the Epilepsy Foundation Washington to honor his leadership and accomplishments over decades. He and his team conduct genetic testing to help diagnose epilepsy syndromes and pinpoint the cause of seizures. This testing also helps families understand the chances of a genetic disorder in subsequent pregnancies. Dr. Novotny’s clinical efforts are closely integrated with ongoing bench research aimed at understanding the cellular mechanisms underlying intractable epilepsy, which involve somatic mutations in the mTOR pathway.
Genetic Breakthrough in Dravet Syndrome
 In breakthrough neuroscience gene therapy research, Franck Kalume, PhD, and colleagues found a novel genetic approach cured Dravet syndrome in a preclinical model. This proof-of-concept study of precision gene therapy targeting GABAergic neurons in the SCN1A gene showed remarkable protection against key symptoms of Dravet syndrome without toxicity or side effects. The study underscored the critical role of precision medicine, as the therapeutic effect relied on selectively targeting a single population of interneurons.
In breakthrough neuroscience gene therapy research, Franck Kalume, PhD, and colleagues found a novel genetic approach cured Dravet syndrome in a preclinical model. This proof-of-concept study of precision gene therapy targeting GABAergic neurons in the SCN1A gene showed remarkable protection against key symptoms of Dravet syndrome without toxicity or side effects. The study underscored the critical role of precision medicine, as the therapeutic effect relied on selectively targeting a single population of interneurons.
Reversing Leigh Syndrome’s Effects
 Alyssa Huff, PhD, Franck Kalume, PhD, Nino Ramirez, PhD, and Christian Arias Reyes, PhD, developed a preclinical model of Leigh syndrome displaying the condition’s typical effects, including disordered swallowing and breathing, and found these effects can be eliminated with chronic exposure to 11% oxygen. Dr. Arias Reyes, a Bolivian researcher, received support through the prestigious Pew Latin American Fellows Program in the Biomedical Sciences to explore how metabolic adaptation to chronic hypoxia can be used to treat Leigh syndrome.
Alyssa Huff, PhD, Franck Kalume, PhD, Nino Ramirez, PhD, and Christian Arias Reyes, PhD, developed a preclinical model of Leigh syndrome displaying the condition’s typical effects, including disordered swallowing and breathing, and found these effects can be eliminated with chronic exposure to 11% oxygen. Dr. Arias Reyes, a Bolivian researcher, received support through the prestigious Pew Latin American Fellows Program in the Biomedical Sciences to explore how metabolic adaptation to chronic hypoxia can be used to treat Leigh syndrome.
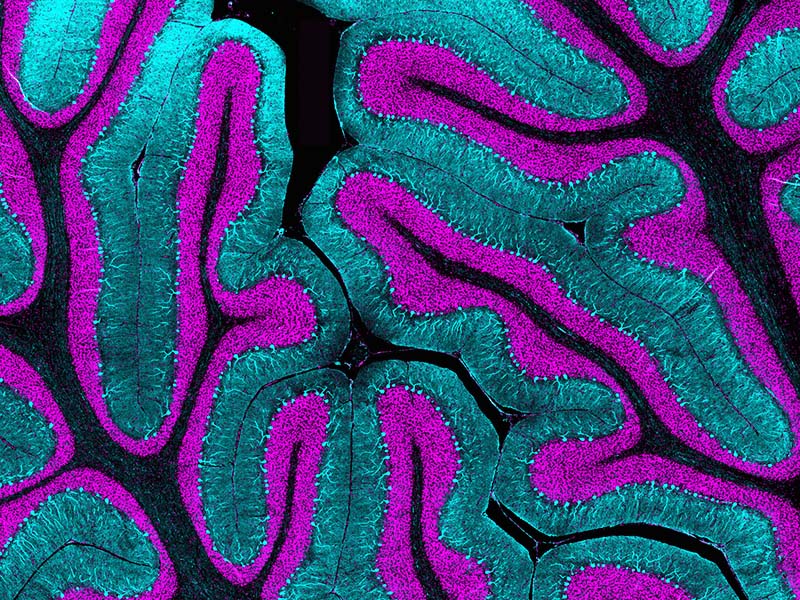
Uncovering the Brain’s Earliest Developments
 Kathleen Millen, PhD, and Parthiv Haldipur, PhD, mapped and described the earliest emergence of neurons in the developing human cerebellum for the first time. Leading the first lab in the world to focus on human cerebellar development, Dr. Millen and colleagues previously identified stem cells in the developing human brain as the cells of origin in pediatric brain tumors, steering global clinical trials for medulloblastoma. Their work highlights key differences between the human brain development and animal models, offering important translational implications.
Kathleen Millen, PhD, and Parthiv Haldipur, PhD, mapped and described the earliest emergence of neurons in the developing human cerebellum for the first time. Leading the first lab in the world to focus on human cerebellar development, Dr. Millen and colleagues previously identified stem cells in the developing human brain as the cells of origin in pediatric brain tumors, steering global clinical trials for medulloblastoma. Their work highlights key differences between the human brain development and animal models, offering important translational implications.
Making Cancer Immunotherapies Safer for Children
 Juliane Gust, MD, PhD, is leading research into how cancer treatment and inflammation affect the developing brain. Dr. Gust measures neurologic injury via blood and cerebrospinal fluid biomarkers in pediatric leukemia patients, uncovers the molecular mechanisms that cause white blood cells to plug capillaries following CAR T cell therapy. Dr. Gust, as well as Stephen Smith, PhD, direct ongoing studies exploring the molecular mechanisms of CAR T cell targeting against brain tumors. With Seattle Children’s at the forefront of pediatric cancer immunotherapy, this research will help deliver lifesaving therapy as safely as possible.
Juliane Gust, MD, PhD, is leading research into how cancer treatment and inflammation affect the developing brain. Dr. Gust measures neurologic injury via blood and cerebrospinal fluid biomarkers in pediatric leukemia patients, uncovers the molecular mechanisms that cause white blood cells to plug capillaries following CAR T cell therapy. Dr. Gust, as well as Stephen Smith, PhD, direct ongoing studies exploring the molecular mechanisms of CAR T cell targeting against brain tumors. With Seattle Children’s at the forefront of pediatric cancer immunotherapy, this research will help deliver lifesaving therapy as safely as possible.
Pinpointing Genetic Causes of Autism
 Damon Page, PhD, has identified two genes, PTEN and Dyrk1a, that cause autism and intellectual disability when mutated. Dr. Page uses preclinical models that allow his lab team to study how the mutations cause atypical brain development so they can develop therapeutics that precisely target the effects of these mutations to improve the quality of life for impacted individuals.
Damon Page, PhD, has identified two genes, PTEN and Dyrk1a, that cause autism and intellectual disability when mutated. Dr. Page uses preclinical models that allow his lab team to study how the mutations cause atypical brain development so they can develop therapeutics that precisely target the effects of these mutations to improve the quality of life for impacted individuals.
Gaining Insights into Pediatric Migraines Through Clinical and Basic Science
 Neurologist Jessica Hauser Chatterjee, MD, PhD, and neuroscientist Franck Kalume, PhD, are investigating a novel SCN1A variant linked to familial hemiplegic migraine, a severe pediatric migraine disorder. Their collaboration began in 2023 when Dr. Kalume presented his work on SCN1A-related epilepsy to the pediatric neurology group. Dr. Hauser Chatterjee, who identified an SCN1A variant in a migraine patient, reached out — and the two quickly found common ground in their shared interest of the gene's role in both migraine and epilepsy. Meeting regularly, they are now building a preclinical model to explore these mechanisms and advance targeted treatment strategies.
Neurologist Jessica Hauser Chatterjee, MD, PhD, and neuroscientist Franck Kalume, PhD, are investigating a novel SCN1A variant linked to familial hemiplegic migraine, a severe pediatric migraine disorder. Their collaboration began in 2023 when Dr. Kalume presented his work on SCN1A-related epilepsy to the pediatric neurology group. Dr. Hauser Chatterjee, who identified an SCN1A variant in a migraine patient, reached out — and the two quickly found common ground in their shared interest of the gene's role in both migraine and epilepsy. Meeting regularly, they are now building a preclinical model to explore these mechanisms and advance targeted treatment strategies.
Featured Researchers
Related Centers & Programs
Pinpointing the Origin of Deadly Brain Tumors
Published
In two papers published in Nature, Dr. Kathleen Millen and her team are the first to identify the cells that give rise to the most aggressive forms of medulloblastoma.
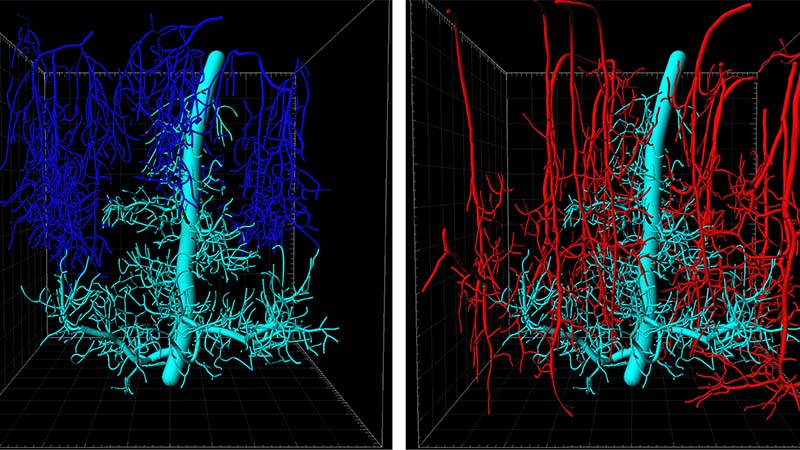
Publication Q&A: Impaired Capillary-Venous Drainage Contributes To Gliosis and Demyelination in White Matter During Aging
Published
Stefan Stamenkovich, PhD, and colleagues investigate the therapeutic effects of capillary drainage within the brain, which has the potential to slow neurological conditions.
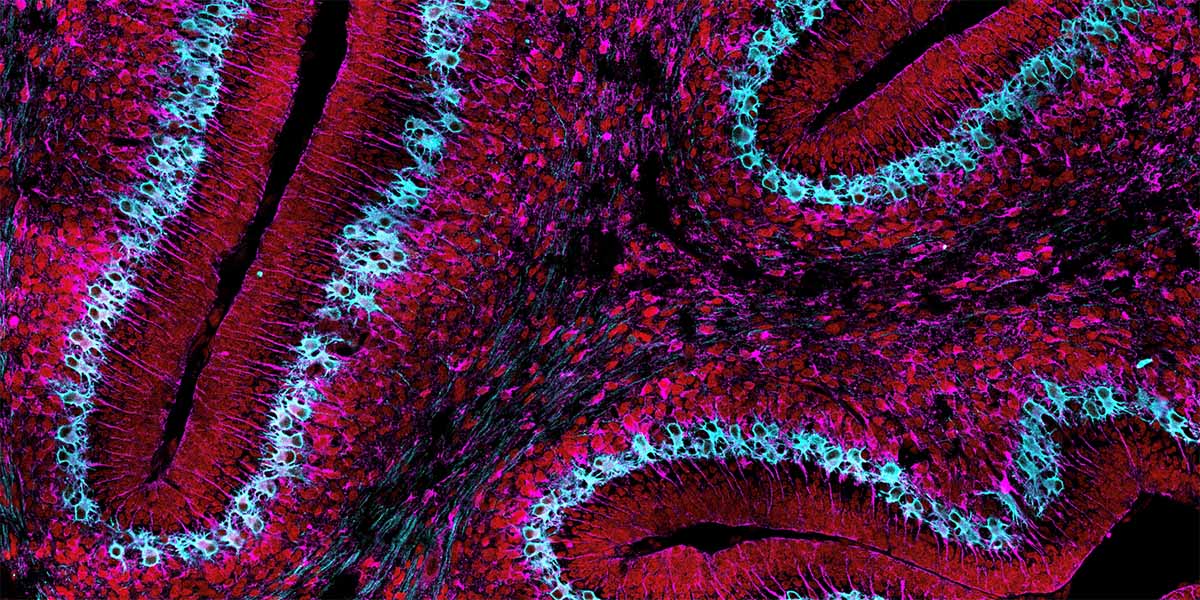
Mapping the Developing Mind: Spatial Transcriptomics Reveals the Early Origin of Bergmann Glia
Published
The Millen Lab solves a 50-year mystery in cerebellar development. Published in PNAS, this research uses spatial transcriptomics to redefine the timeline of Bergmann glia and correct long-standing inaccuracies in brain science.