Tricuspid Atresia
What is tricuspid atresia?
Tricuspid atresia (try-CUSP-id ah-TREE-sha) is a complex, congenital birth defect in which a baby’s heart does not have a tricuspid valve.
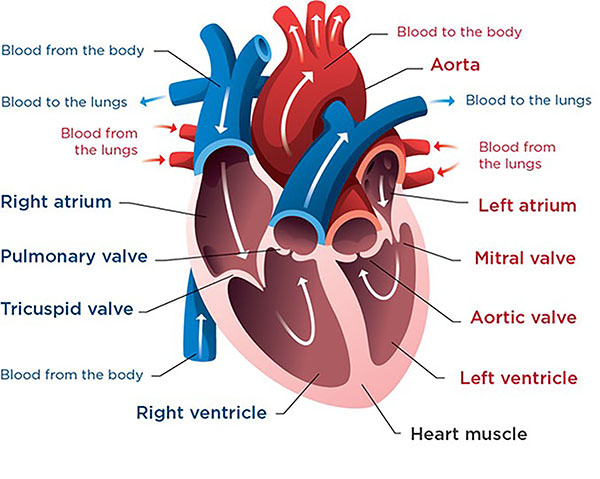 This is a healthy heart. The tricuspid valve lets blood flow from the right atrium into the right ventricle to get pumped to the lungs.
This is a healthy heart. The tricuspid valve lets blood flow from the right atrium into the right ventricle to get pumped to the lungs.In normal hearts, the tricuspid valve is the door that allows blue (oxygen-poor) blood to flow from the right atrium of the heart into the right ventricle. The right ventricle then pumps the blood through the pulmonary artery to the lungs to pick up oxygen.
In babies with tricuspid atresia, the tricuspid valve does not form. There is no opening to let blood travel directly from the right atrium into the right ventricle.
These babies typically pump some blood to their lungs by a different route. Even so, the oxygen level in their blood is lower than normal, so their body does not get as much oxygen as it needs (cyanotic heart disease). Also, their right ventricle often does not grow the way it should and is smaller than normal.
Most babies with tricuspid atresia need treatment in the first days or weeks of life.
-
Blood flow in babies with tricuspid atresia
 From heart.org. ©2009, American Heart Association, Inc.
From heart.org. ©2009, American Heart Association, Inc.In babies with tricuspid atresia, the only way for blood to get out of their right atrium is through a hole in the wall between the right and left atria (atrial septal defect, ASD). Most babies with tricuspid atresia also have a hole in the wall between the right and left ventricles (ventricular septal defect, VSD).
With tricuspid atresia, blue (oxygen-poor) blood comes from the body into the right atrium. Then, it passes through the ASD into the left atrium, where it mixes with red (oxygen-rich) blood. This mixed (purple) blood then flows into the left ventricle, which pumps it through the aorta to the brain and body. If the baby has a VSD, some of the mixed blood passes through the VSD into the right ventricle, which pumps it through the pulmonary artery to the lungs.
Some of the blood that enters the aorta gets channeled through a blood vessel called the ductus arteriosus. This vessel joins the aorta to the pulmonary artery. It provides another way for some blood to get to the lungs.
Usually, the ductus arteriosus closes soon after birth. In newborns with tricuspid atresia, the ductus arteriosus may be the only way for blood to reach their lungs. For this reason, doctors may start giving a medicine called prostaglandin right after birth to keep the ductus arteriosus open.
-
Other heart problems related to tricuspid atresia
Some babies with tricuspid atresia have other conditions that also affect blood flow through their heart. These may include pulmonary stenosis or transposition of the great arteries. Both of these conditions can complicate the diagnosis and affect the type of surgery a baby needs.
Heart Center at Seattle Children's
What are the symptoms of tricuspid atresia?
Most babies with tricuspid atresia show symptoms within the first few hours after birth. In some babies, it may take a few days or weeks for symptoms to appear.
Symptoms of tricuspid atresia may include:
- Heart murmur (the sound of blood moving in the heart in a way that’s not normal)
- Skin may look blue or purple tinged, mottled (different shades or colors), grayish or paler than usual; the lips, mouth, gums, fingernails or toenails may look bluish (cyanosis)
- Fast breathing
- Working hard to breathe
- Poor feeding
- Poor weight gain or growth
How is tricuspid atresia diagnosed?
Usually, doctors diagnose tricuspid atresia when a baby is in the womb using a fetal echocardiogram (fetal echo). This is a special ultrasound that uses sound waves to view and make pictures of a developing baby’s heart during pregnancy. The results are interpreted by a pediatric heart doctor (cardiologist) who specializes in fetal congenital heart disease.
Your obstetrician may refer you for a fetal echo if your family has a history of congenital heart disease or if a routine prenatal ultrasound shows a problem.
Seattle Children’s Fetal Care and Treatment Center team can care for you when you are pregnant if your developing baby has a known or suspected problem. A team that includes cardiologists and heart surgeons will work together to plan and provide the treatment your baby will need when they are born.
After birth, your baby may need 1 or more of these tests to get more details about their condition:
- ECG or EKG (electrocardiogram)
- Echocardiogram
- Blood tests
- Chest X-rays
- Cardiac catheterization
How is tricuspid atresia treated?
The doctor will likely suggest some procedures and treatments right away after your baby is born to improve your baby’s blood flow. Other procedures may be done later, such as open-heart surgery. Most babies can be helped with surgery.
We provide complete care for children with tricuspid atresia through our Single Ventricle Program. We will coach you on how to check your baby’s condition at home, and we will give you 24-hour support in case problems arise. This helps us find small issues before they become serious problems.
Medicine
The doctor may give your baby medicine (prostaglandin) to help keep the ductus arteriosus from closing and to help the blood flow. Doctors give this medicine through an intravenous (IV) line.
Catheterization
Your baby may need cardiac catheterization with a balloon to make the opening between their atria large or with a stent to keep the ductus arteriosus open.
Surgery
Your baby will likely need several surgeries done in stages during the first few years of life to improve their blood flow. The exact procedures and timing depend on your child’s diagnosis, heart anatomy and symptoms. The surgical team at Seattle Children’s will talk with you in more detail about your child’s needs.
The most common surgeries are:
-
Blalock-Thomas-Taussig shunt
Keeping the ductus arteriosus open with medicine is a good short-term way to get blood to the lungs. But often, babies need a more lasting connection. This is called a Blalock-Thomas-Taussig (BTT) shunt.
The BTT shunt is a small plastic tube that connects the aorta (blood supply to the body) and the pulmonary artery (blood supply to the lungs). A surgeon sews the tube in place, or a shunt can be placed in a cardiac catheterization procedure.
If your baby needs a shunt, we do this soon after birth — typically in the first 1 to 2 weeks. After this surgery, the oxygen levels in the body will still be lower than normal, usually around 80%.
-
Bidirectional Glenn
The bidirectional Glenn is a surgery that changes blood flow from a large vein called the superior vena cava. Normally, this vein carries blue (oxygen-poor) blood from the upper part of the body into the heart, which pumps the blood to the lungs. After the surgery, the blue blood flows to the lungs without going through the heart first.
Newborns cannot have this surgery because the blood pressure in their lungs is too high. We usually do this surgery around age 3 to 6 months, when the blood pressure in the lungs has reached its normal low level. After this surgery, the oxygen level in the body will still be lower than normal, usually around 80%.
This surgery is sometimes called the hemi-Fontan.
-
Fontan
The final planned surgery for tricuspid atresia is called the Fontan operation. This surgery changes blood flow from a large vein called the inferior vena cava. Normally, this vein carries blue blood from the lower part of the body into the heart, which pumps it to the lungs. After the surgery, all the blue blood returning from the body flows to the lungs without going through the heart first.
When the Fontan surgery is done, the flow of blood to the lungs is completely separate from the flow to the body. The oxygen level in the body is normal, usually greater than 95%. After your child has a Fontan procedure, they get coordinated, ongoing, team-based care through our Fontan Clinic.
Children with tricuspid atresia need lifelong follow-up care for their heart.
Tricuspid Atresia at Seattle Children’s
-
The experts you need are here
- The Heart Center team includes more than 40 pediatric cardiologists who diagnose and treat every kind of heart problem. We have treated many children with tricuspid atresia.
- Our doctors and surgeons are experts in the treatments your child may need, including cardiac catheterizations and surgery. Seattle Children’s outcomes for surgeries to change the flow of blood to the heart and lungs are among the best in the nation.
- Children with tricuspid atresia receive comprehensive care through our Single Ventricle Program.
- We also have a pediatric cardiac anesthesia team and Cardiac Intensive Care Unit for children who need them. General anesthesia is a medicine we give to people before surgery so they are fully asleep during the procedure.
- Your child’s team includes other experts from Seattle Children’s based on their needs, like neonatologists and pulmonologists.
-
Care from before birth through young adulthood
- Most developing babies with tricuspid atresia are diagnosed before birth. If this happens, Seattle Children’s Fetal Care and Treatment Center team works closely with you and your family to plan and prepare for any care your baby may need.
- Your child’s treatment plan is custom-made. We plan and carry out their treatment based on the specific details of their heart condition. We closely check your child’s needs to make sure they get the care that is right for them at every age.
- We have a special Adult Congenital Heart Disease Program to meet your child’s long-term healthcare needs. This program, shared with the University of Washington, transitions your child to adult care when they are ready.
-
Support for your whole family
- We are committed to your child’s overall health and well-being and to helping your child live a full and active life.
- Whatever types of care your child needs, we will help your family through this experience. We will discuss your child’s condition and treatment options in ways you understand and involve you in every decision.
- Our Child Life specialists know how to help children understand their illnesses and treatments in ways that make sense for their age.
- Seattle Children’s has many resources, from financial to spiritual, to support your child and your family and make your experience as smooth as possible.
- Many children and families travel to Seattle Children’s for heart surgery or other care. We help you coordinate travel and housing so you can stay focused on your child.
- Read more about the supportive care we offer.
Contact Us
Contact the Heart Center at 206-987-2515 for an appointment, second opinion or more information.
Providers, see how to refer a patient.
Related Links
- Heart Center
- Heart Surgery
- Heart Center Team
- Single Ventricle Program
- Statistics and Outcomes
- Cardiac Catheterization Procedures
Paying for Care
Learn about paying for care at Seattle Children’s, including insurance coverage, billing and financial assistance.


