Patent Ductus Arteriosus
What is patent ductus arteriosus?
 From heart.org. ©2009, American Heart Association, Inc.
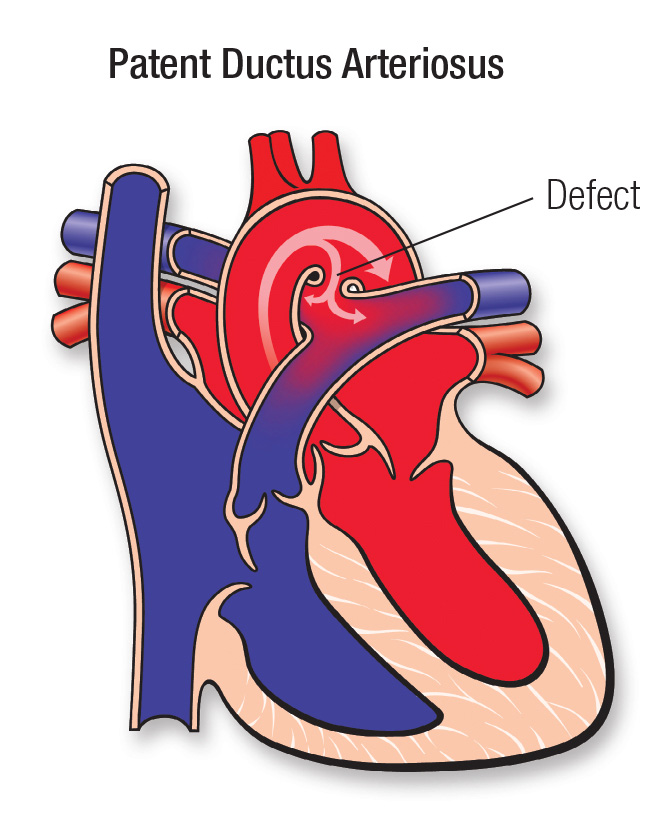
From heart.org. ©2009, American Heart Association, Inc.The ductus arteriosus (DUCK-tus are-teer-e-OH-sis) is a blood vessel that babies have before they are born. It connects the pulmonary artery to the aorta and lets most blood leave the heart without going through the lungs.
This works fine because babies do not breathe on their own until after birth. Before they are born, babies do not need much blood going to their lungs to get oxygen. Instead, they get oxygen through the placenta.
The ductus typically closes within a few days after birth. If it stays open, it is called a patent ductus arteriosus (PAY-tent DUCK-tus are-teer-e-OH-sis), or PDA. If this happens, pressure from the blood vessels will send extra blood to the lungs. This extra blood then returns to the heart and can cause the heart’s left side to become too large. If not treated, this could lead to heart failure.
Some babies with PDA have other heart defects.
Who gets patent ductus arteriosus?
A ductus that does not close is common in premature babies. Researchers estimate that 1 in 5 to 3 in 5 premature babies have PDA. It can also happen in full-term babies, but this is much less common.
This condition happens more often in:
- Babies with trisomy 13 (Patau syndrome), trisomy 18 (Edwards syndrome) or trisomy 21 (Down syndrome)
- Babies with Holt-Oram syndrome or Noonan syndrome
- Babies born to someone who had German measles (rubella) while pregnant
Why might doctors want to keep the ductus open?
If your baby’s ductus is closing in the normal way after birth but they have other heart defects (like hypoplastic left heart syndrome, interrupted aortic arch or pulmonary atresia), doctors may want to keep the ductus open. To do this, they give your baby medicine (prostaglandin). This step helps blood flow through your baby’s heart and into the rest of their body until they can have treatment for other heart defects.
Heart Center at Seattle Children's
Symptoms of Patent Ductus Arteriosus
If your child’s ductus arteriosus does not close, they may not have any symptoms unless their heart and lungs are getting too much blood because the ductus is large.
If your child does have symptoms, they may include:
- Fast breathing and fast heartbeat
- Working hard to breathe
- Trouble feeding
- Poor weight gain or slow growth (failure to thrive)
- Getting more tired than normal
- Sweating
Diagnosing Patent Ductus Arteriosus
To diagnose this condition, your child’s doctor will examine your child and listen to their heart. Sometimes, doctors find PDA after hearing a heart murmur in a child who appears well. They may not hear a murmur and not find the ductus problem until the child is older.
To get more information about your child’s heart, the doctor may ask for tests, including:
- Echocardiogram
- Electrocardiogram (ECG or EKG)
Treating Patent Ductus Arteriosus
PDA may close on its own over time. This is more common in premature babies.
If your child’s ductus is small and not causing problems, their doctor may suggest waiting to see if it closes in their first year or 2.
If the ductus is moderate or large, it is likely to cause problems (or may have already caused problems) with your child’s blood flow, breathing or heart function. The doctor may suggest taking steps to close it.
Medicine
If your baby is premature, doctors may use medicines (indomethacin or ibuprofen) to close the ductus.
Catheterization
In premature babies, full-term babies and children, doctors can usually close the ductus arteriosus with a cardiac catheterization procedure. The doctor uses a small, thin tube (catheter), inserted through a blood vessel in the leg, to close the ductus arteriosus. Your child will be given general anesthesia for this procedure, so they will be fully asleep.
Surgery
Some premature infants and children may need surgery if their ductus arteriosus is too large to close with cardiac catheterization.
Patent Ductus Arteriosus at Seattle Children’s
-
The experts you need are here
- The Heart Center team includes more than 40 pediatric cardiologists who diagnose and treat every kind of heart problem. We have treated many children with patent ductus arteriosus.
- Our doctors and surgeons are experts in the treatments your child may need, including medicine, cardiac catheterization or surgery.
- We also have a pediatric cardiac anesthesia team, Cardiac Intensive Care Unit and newborn (neonatal) intensive care doctors for children who need them.
- Your child’s team includes other experts from Seattle Children’s based on their needs, like doctors who specialize in lung health (pulmonologists).
-
Care from birth through young adulthood
- Your child’s treatment plan is custom-made. We plan and carry out their treatment based on the specific details of their heart defect. We closely check your child’s needs to make sure they get the care that is right for them at every age.
- We have a special Adult Congenital Heart Disease Program to meet your child’s long-term healthcare needs. This program, shared with the University of Washington, transitions your child to adult care when they are ready.
-
Support for your whole family
- We are committed to your child’s overall health and well-being and to helping your child live a full and active life.
- Whatever types of care your child needs, we will help your family through this experience. We will discuss your child’s condition and treatment options in ways you understand and involve you in every decision.
- Our Child Life specialists know how to help children understand their illnesses and treatments in ways that make sense for their age.
- Seattle Children’s has many resources, from financial to spiritual, to support your child and your family and make the journey as smooth as possible.
- Many children and families travel to Seattle Children’s for heart surgery or other care. We help you coordinate travel and housing so you can stay focused on your child.
- Read more about the supportive care we offer.
-
Advancing treatment for children
- We take part in multicenter studies to learn more about the best care options for children with PDAs and to improve their outcomes.
- Our doctors and patients were part of a national study that led to approval of the Piccolo Occluder in premature infants and newborns. Doctors can thread this device into the heart of small babies to close (block) the ductus. We now use this option on a regular basis.
Contact Us
Contact the Heart Center at 206-987-2515 for an appointment, second opinion or more information.
Providers, see how to refer a patient.
Related Links
- See a picture (American Heart Association)
- Cardiac Catheterization Procedures
- Heart Center
- Heart Surgery
Paying for Care
Learn about paying for care at Seattle Children’s, including insurance coverage, billing and financial assistance.


