Double-Inlet Left Ventricle
What is double-inlet left ventricle?
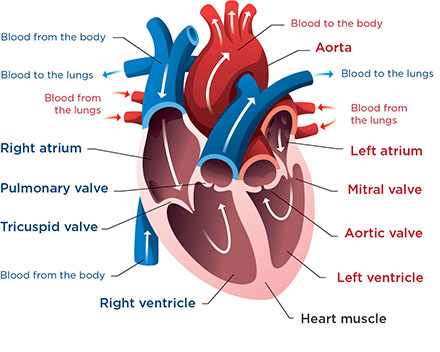 This is a normal heart. In double-inlet left ventricle, both the mitral valve and the tricuspid valve lead into the left ventricle. The right ventricle is small and not well developed.
This is a normal heart. In double-inlet left ventricle, both the mitral valve and the tricuspid valve lead into the left ventricle. The right ventricle is small and not well developed.Double-inlet left ventricle is a birth defect in the heart.
Normally, the mitral valve leads into the heart’s left pumping chamber (ventricle), and the tricuspid valve leads into the right ventricle.
In babies with this defect, both the mitral valve and the tricuspid valve lead into the left ventricle. This lets oxygen-rich (red) and oxygen-poor (blue) blood mix in the heart and get pumped out to your child’s body. Only the left ventricle works. The right ventricle is small and not well developed. It cannot pump blood to the lungs like it typically would.
Children with this defect may have other heart problems, too, like transposition of the great arteries, coarctation of the aorta, pulmonary atresia or pulmonary stenosis.
What causes double-inlet left ventricle?
This is a congenital defect. Doctors do not know why it happens. They think it occurs early in the pregnancy when the baby’s heart is forming.
How common is double-inlet left ventricle?
About 5 in every 100,000 babies have double-inlet left ventricle. Doctors consider it a rare heart defect.
Heart Center at Seattle Children's
What are the symptoms of double-inlet left ventricle?
Your child may have symptoms like these:
- Getting tired easily
- Blue or purple-tinged skin, lips or fingernails (cyanosis) or skin that looks mottled, grayish or paler than your baby’s usual skin color
- Trouble feeding
- Trouble gaining weight and growing
- Fast breathing or working hard to breathe
- Sweating more than normal
- Swelling (edema) in the legs and abdomen
How is double-inlet left ventricle diagnosed?
-
Fetal diagnosis
Usually, doctors can diagnose double-inlet left ventricle when a baby is in the womb using a fetal echocardiogram (fetal echo). This is a special ultrasound that uses sound waves to view and make pictures of a developing baby’s heart during pregnancy. The results are interpreted by a pediatric heart doctor (cardiologist) who specializes in fetal congenital heart disease.
Your obstetrician may refer you for a fetal echo if your family has a history of congenital heart disease or if a routine prenatal ultrasound shows a problem.
Seattle Children’s Fetal Care and Treatment Center team can care for you when you are pregnant if your developing baby has a known or suspected problem.
-
Diagnosis in newborns
To diagnose this condition, your child’s doctor will examine your baby, check their heartbeat and pulse and listen to their heart. In children with double-inlet left ventricle, doctors can often hear a heart murmur — the sound of blood moving in the heart in a way that’s not normal.
The doctor will ask for details about your child’s symptoms, their health history and your family health history.
Your child will need tests that provide more information about how their heart looks and works. These may include:
- Chest X-rays
- Cardiac catheterization
- MRI (magnetic resonance imaging)
- Echocardiography
- Electrocardiography
How is double-inlet left ventricle treated?
Babies with double-inlet left ventricle need surgery in the first weeks of life. They get a series of surgeries to change blood flow through their heart.
This condition is called a “single-ventricle heart defect” because there is only 1 pumping chamber in the heart, instead of the usual 2. Single-ventricle defects are some of the most complex heart birth defects. We provide comprehensive care for children with double-inlet left ventricle through our Single Ventricle Program. Those who have a Fontan procedure get coordinated, ongoing, team-based care through our Fontan Clinic.
-
Surgery
Babies born with double-inlet left ventricle usually have 3 surgeries during the first few years of life to change the blood flow through their heart:
- Oxygen-poor blood, which returns from the body, is sent to blood vessels that go to the lungs.
- Oxygen-rich blood returns from the lungs into the working ventricle. This ventricle should be able to pump the oxygen-rich blood to the entire body.
The exact procedures and timing depend on your child’s condition and any other heart defects they have.
-
Medicine
Your child may need medicines like these before and after surgery:
- Angiotensin-converting enzyme (ACE) inhibitors, which lower blood pressure
- Digoxin, which makes the heart beat slower and with more force
- Anticoagulants, which help prevent or dissolve blood clots
-
Transplant
Some children need a heart transplant. The heart transplant team at Seattle Children’s does many transplants each year for children with this or other heart problems that cannot be controlled with standard medical or surgical treatment. Read more about our Heart Transplant Program and our exceptional outcomes.
-
Follow-up care
Outcomes for children with double-inlet left ventricle have improved greatly in the past several decades. Still, these babies are quite vulnerable between their first and second surgeries. They are at risk for serious health problems from common childhood illnesses, like colds, and they may have trouble feeding and growing. To provide care and closely check babies with double-inlet left ventricle, we see them through our Single Ventricle Program.
Why choose Seattle Children's for double-inlet left ventricle treatment?
-
The experts you need are here
- The Heart Center team includes more than 40 pediatric cardiologists who diagnose and treat every kind of heart problem. We have treated many babies with this condition.
- Our doctors and surgeons are experts in the treatments your child may need. These may include surgery to change blood flow in your child’s heart, medicine and a heart transplant.
- Our 4 pediatric cardiac surgeons perform more than 500 procedures yearly. Our surgical outcomes are among the best in the nation year after year. See our outcomes for surgeries related to single-ventricle defects.
- We also have a pediatric cardiac anesthesia team and a Cardiac Intensive Care Unit ready to care for children who have heart surgery.
- Children with double-inlet left ventricle receive compassionate, comprehensive care through Seattle Children’s Single Ventricle Program. We bring together specialists in cardiology, nutrition, social work, feeding therapy and neurodevelopment to support your child’s health between surgeries.
- The transplant team does several heart transplants each year for children with this or other heart problems that cannot be controlled using other treatments.
- Your child’s team includes experts from other areas of Seattle Children’s based on their needs, like doctors who specialize in newborns (neonatologists) or lung health (pulmonologists).
-
Care from fetal diagnosis through young adulthood
- If your developing baby is diagnosed with double-inlet left ventricle before birth, our Fetal Care and Treatment Center team works closely with you and your family to plan and prepare for any care your baby may need.
- Your child’s treatment plan is custom-made. We plan and carry out their treatment based on the specific details of their heart defect. We closely check your child’s needs to make sure they get the care that is right for them at every age.
- We have a special Adult Congenital Heart Disease Program to meet your child’s long-term healthcare needs. This program, shared with the University of Washington, transitions your child to adult care when they are ready.
-
Support for your whole family
- We are committed to your child’s overall health and well-being and to helping your child live a full and active life.
- Whatever types of care your child needs, we will help your family through this experience. We will discuss your child’s condition and treatment options in ways you understand and involve you in every decision.
- Our Child Life specialists know how to help children understand their illnesses and treatments in ways that make sense for their age.
- Seattle Children’s has many resources, from financial to spiritual, to support your child and your family and make the journey as smooth as possible.
- Many children and families travel to Seattle Children’s for heart surgery or other care. We help you coordinate travel and housing so you can stay focused on your child.
- Read more about the supportive care we offer.
-
Advancing treatment for children
Seattle Children’s is part of a nationwide group of children’s hospitals called the National Pediatric Cardiology Quality Improvement Collaborative (NPC-QIC). This group works to improve the outcomes and quality of life for children with double-inlet left ventricle. The NPC-QIC also offers resources, support and information for families.
Patient story: Luke isn’t defined by his heart defect (Video. 2:06)
Years after Luke was treated for double-inlet left ventricle, his mom, Jesse, thinks her thriving son may get his curiosity and thirst for details from his early experience with medical care.
Contact Us
Contact the Heart Center at 206-987-2515 for an appointment, second opinion or more information.
Providers, see how to refer a patient.
Related Links
- Heart Center
- Heart Center Team
- How to Handle a Difficult Prenatal Diagnosis
- What to Expect: Heart Surgery
Paying for Care
Learn about paying for care at Seattle Children’s, including insurance coverage, billing and financial assistance.


