Immunology Research Progress Shared at Cell and Gene Therapy Annual Meeting
Published
Novel cell and gene therapies created at Seattle Children’s Research Institute with the potential to more efficiently treat or cure lupus, hemophilia A, brain cancer, congenital neutropenia and more will be showcased at the American Society of Gene and Cell Therapy’s (ASGCT) Annual Meeting, May 13 to 17, in New Orleans.
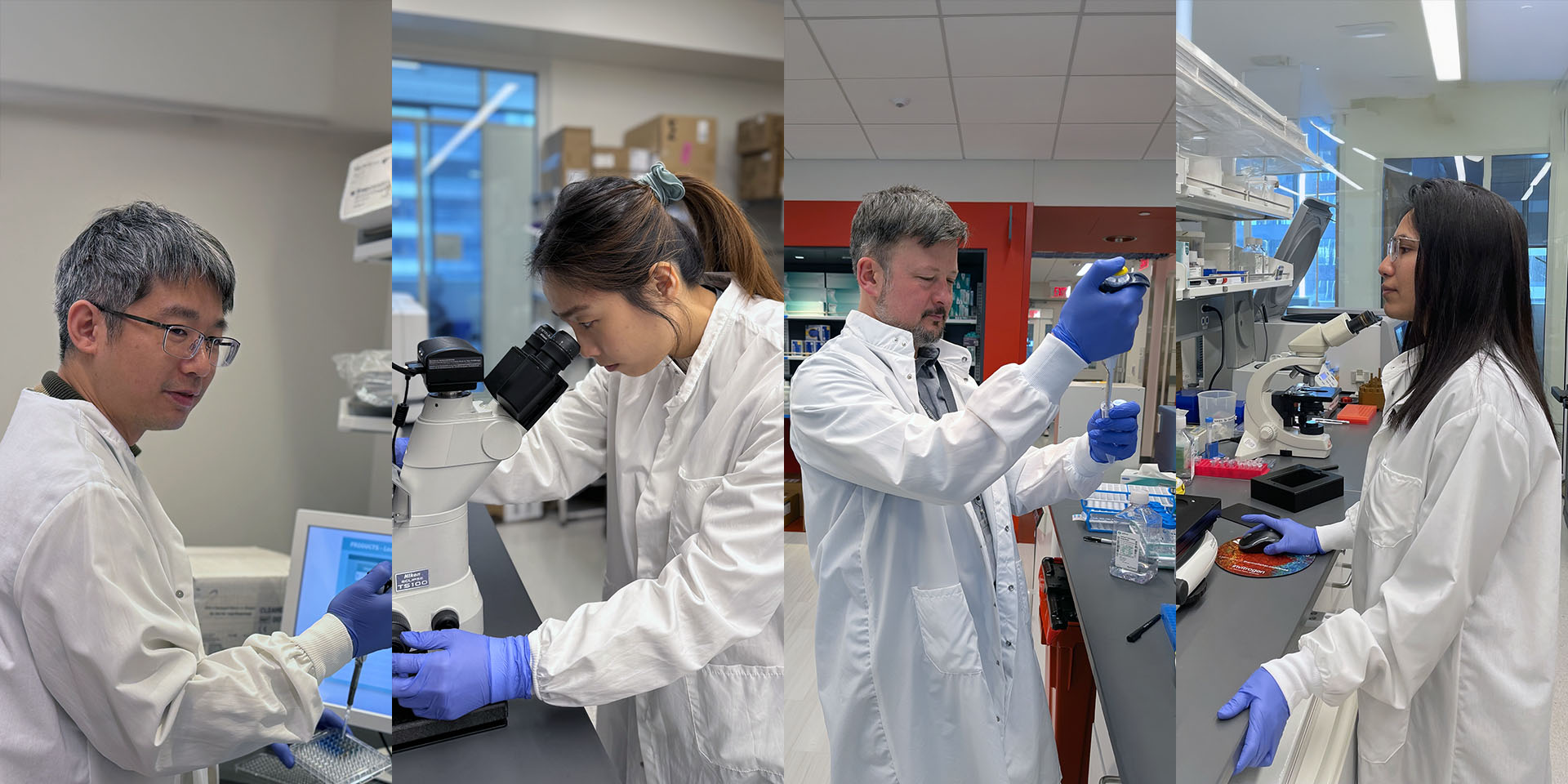
Twelve oral and poster abstracts are being presented by 11 Children’s scientists to the over 8,000 researchers from around the world expected to attend the conference. Only a small percentage of submissions are chosen for presentations each year, but Children’s entries are reliably selected, reflecting the leadership role of Seattle Children’s in this field.
It’s a point of pride for David Rawlings, MD, director of the research institute’s Center for Immunity and Immunotherapies: “The center consistently has abstracts chosen for presentation at the annual meeting, including oral presentations, which comprise a very small percentage of the more than 1,000 submitted abstracts,” he said.
“ASGCT is the premier international meeting on cell and gene therapy,” Dr. Rawlings said. “It permits [Seattle Children’s] to present our newest data to a large, highly engaged audience, and it allows networking with other academic research groups, as well as industry and biotech leaders.”
Children’s researchers’ abstracts highlight rapid progress in expanding novel gene and cell therapy platforms invented at the research institute. “The incredible team effort behind this work should be recognized and celebrated. These abstracts reflect the collaborative dedication of entire labs,” said Sowmya Pattabhi, PhD, director of Seattle Children’s Therapeutics’ Correlative Sciences Lab.
Five Children’s researchers are sharing their findings at prestigious oral abstract sessions:
Safer, More Effective Treatments for Genetic Disorders
“We discovered a new method to treat hemophilia A using ultrasound and microbubbles to deliver the necessary gene. This approach proved effective in studies of a preclinical model, showing lasting results with minimal side effects. This research could lead to safer, more effective treatments for genetic disorders, reducing the need for frequent and costly therapies.”
—Ting-Yen (Scott) Chao, research scientist, Miao Lab, Center for Immunity and Immunotherapies
New Tests to Detect Cancer-Fighting Cells
“We developed a new test that can detect and measure special cancer-fighting cells in very small amounts in a patient's cerebrospinal fluid. This test helps us better understand how treatments are working and why some patients respond differently than others. We want to know which cancer-targeting molecules remain in the brain after treatment, and how can measuring them improve future therapies?”
—Audrey Alderman, research scientist, Correlative Sciences Lab, Seattle Children’s Therapeutics
Better Brain Tumor Therapy
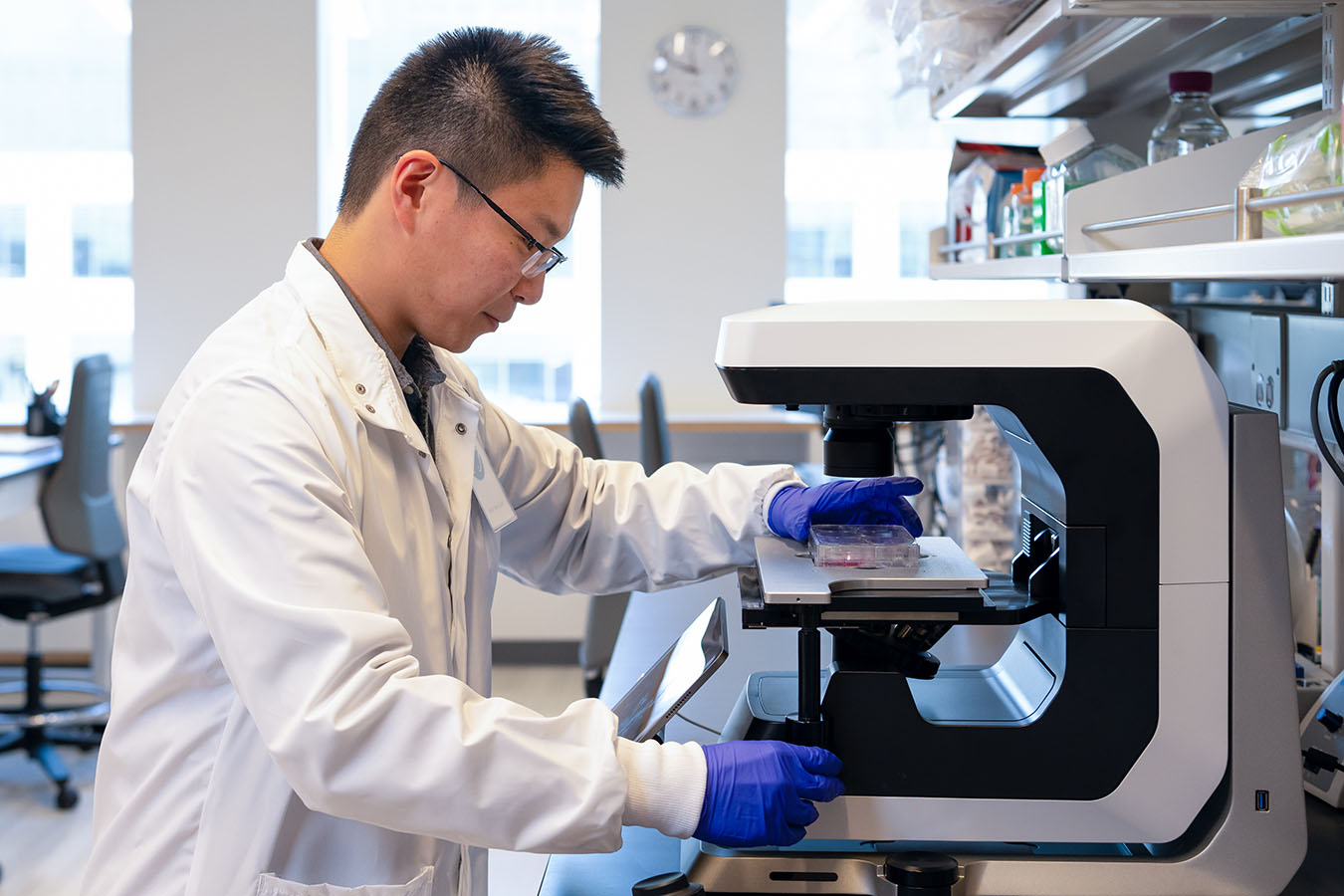
“We improved our CAR T cell technology with an additional gene modification so that the tumor-killing CAR T cells could more efficiently locate and travel to the tumors, and we showed that these enhanced CAR T cells were more effective in treating preclinical models with pediatric brain tumors. We hope this new iteration of CAR T cell technology can bring cures to children with brain tumors and save invaluable lives.”
—Edward Song, PhD, Invent at Seattle Children’s postdoctoral scholar in the Vitanza Lab, Ben Towne Center for Childhood Cancer and Blood Disorders Research

Modulating Autoimmune Responses
“We used gene editing to turn human T cells into engineered regulatory T cells (EngTregs) that target and suppress the B cells responsible for producing the harmful antibodies seen in lupus and other autoimmune diseases. These EngTregs lowered antibody production in lab tests and resulted in reduced inflammatory signals in a preclinical model compared to current therapies.”
—Annaiz Grimm, research scientist, Rawlings Lab, Center for Immunity and Immunotherapies
Correcting congenital conditions
“We tested a new gene therapy method for the treatment of congenital neutropenia disorders using patient cells. We utilized a novel gene editing approach designed to eliminate only the mutant gene copy that causes the disease while leaving a healthy copy intact. Following editing of patient bone marrow stem cells and transplantation into a preclinical model, we show correction of the disease long term.”
—Aidan Laird, research scientist, Rawlings Lab, Center for Immunity and Immunotherapies
Research Progress Toward Safer Hemophilia A Treatments
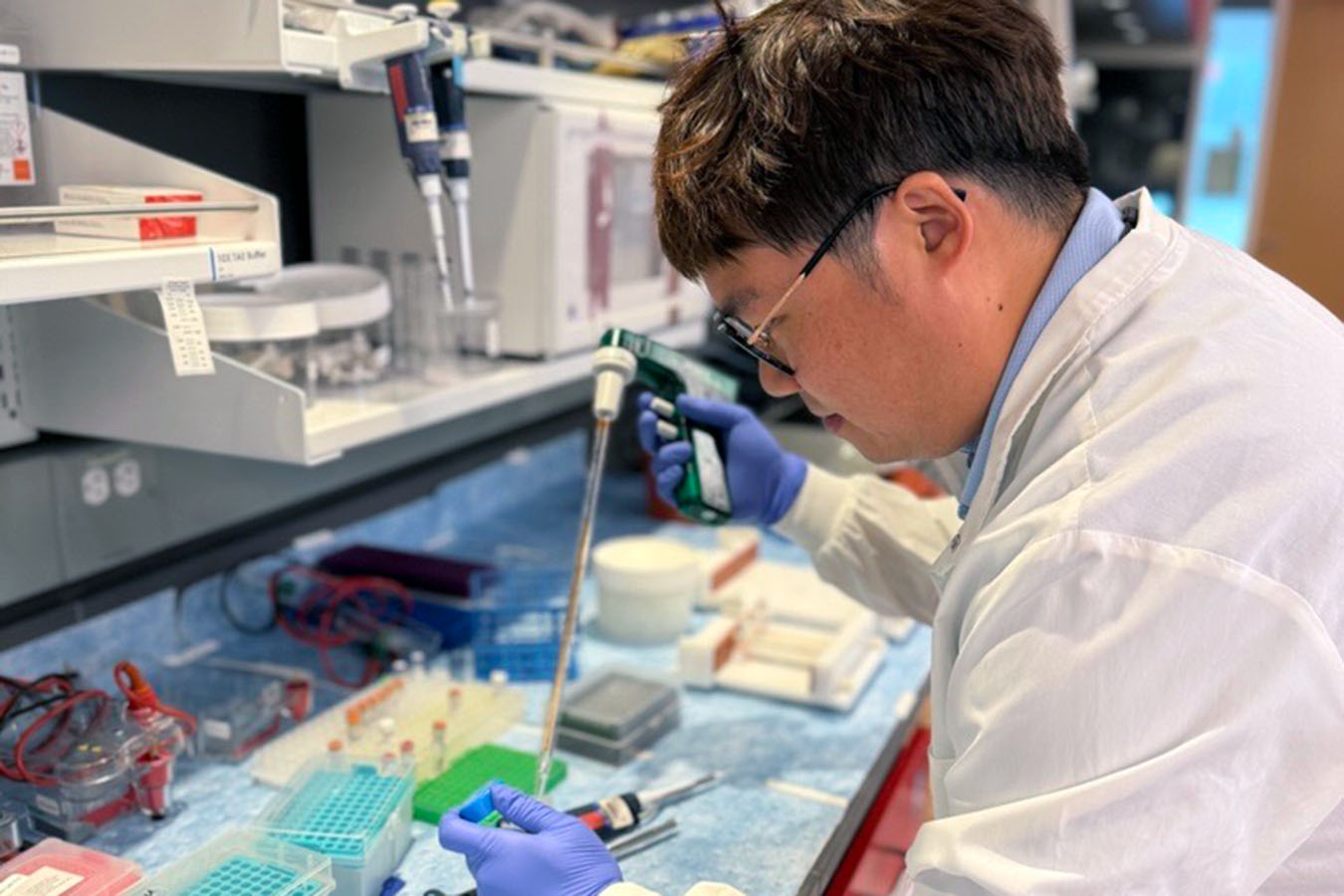
Three poster presentations from research scientists on the Miao Lab team show progress toward safer, more effective treatments for hemophilia A, a genetic disorder where the blood doesn't clot properly due to lack of a protein called factor VIII (FVIII).
Chun-Yu Chen and colleagues developed a novel CRISPR/Cas9-based strategy to repair the missing exon of the FVIII gene in a preclinical model of hemophilia A. This gene repair would allow patients to make the protein needed to stop bleeding and help wounds heal properly.
Meng-Ni Fan and team are experimenting with a lipid nanoparticle-based non-viral delivery of FVIII to treat the blood-clotting disorder. The treatment lasted for many months and could be given again safely, offering hope for a new type of gene therapy. The research could pave the way for safer and repeatedly administered gene therapies, making these treatments more accessible for various genetic disorders that require long-term intervention.
Ting-Yen (Scott) Chao and collaborators are asking: Can ultrasound-mediated gene delivery effectively and safely treat hemophilia A by fixing the faulty gene? They used ultrasound and microbubbles to deliver CRISPR/Cas9 gene-editing tools in preclinical models, fixing the faulty gene and restoring some clotting ability.
“As an abstract reviewer for ASGCT, I can attest that the high acceptance rate of our abstracts indicates the high quality and excellence of the scientific advances from Children’s researchers,” said principal investigator Carol Miao, PhD, who is co-chairing two oral abstract sessions and a scientific symposium at this year’s meeting.
Cell Therapy Advances in Solid Tumor Therapies, Immune System Reprogramming, and B Cell Biology
Other Children’s poster presenters share research insights into creating better solid tumor therapies, reprogramming the immune system to halt autoimmune diseases, and better understanding B cell biology.
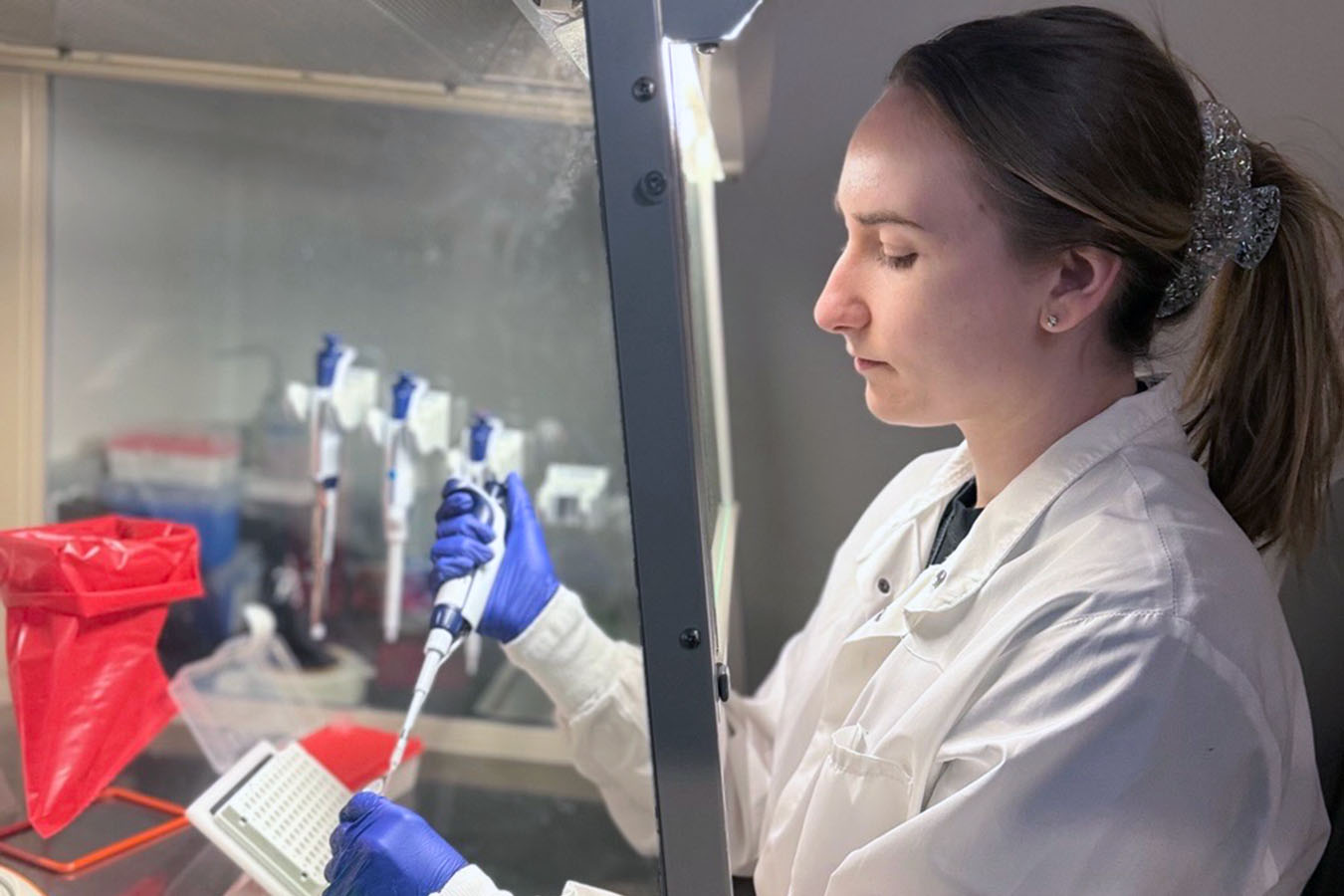
Miranda Lyons-Cohen, PhD, an Invent at Seattle Children’s postdoctoral scholar, and graduate student Simonne Guenette, both in the Ben Towne Center’s Oda Lab, are each presenting posters on development of next-generation cell therapies to treat pediatric cancers. They and their team are engineering strategies that enable T cells to overcome obstacles in the tumor microenvironment and mount a more powerful, durable and sustained attack on cancer cells by replacing a T cell brake with an accelerator.
Using Engineered Regulatory T Cells to Treat Autoimmune Disease (CGTlive.com)
To treat disorders involving pathogenic antibodies, including lupus and organ transplant rejection, Peter Cook, a research scientist in the Rawlings Lab, and colleagues have developed a new type of cell-based medicine that can target and kill the plasma cells that secrete problematic antibodies. Such an approach could stop the immune system from attacking healthy tissues in autoimmune diseases like type 1 diabetes and multiple sclerosis and reduce the chance of rejection in solid organ transplantation.
“ASGCT offers the opportunity to see the broader scope of the field and get a sense of different technologies that are being developed within the cell and gene therapy space,” Cook said. “We can see the real benefit these therapies are providing to patients in the form of clinical trial data that is frequently presented at the meeting.”
Nikita Trivedi, a research scientist in the Center for Immunity and Immunotherapies’ James Lab, analyzed the role of integrins — proteins that facilitate cell-to-cell communication — in antibody-producing human plasma cells in a preclinical model, revealing that two key integrins are partially required for plasma cells to localize to the bone marrow, challenging previous assumptions. However, enhancing their expression with retinoic acid directed plasma cells to abdominal fat, offering potential for site-specific B cell therapeutic delivery.
Principal investigator Rich James, PhD, is excited for Nikita and others to share their findings at ASGCT. “Our team members will get specific feedback on their presentations from experts from a diverse set of fields/perspectives, and this helps guide and prioritize future studies,” he said.
“At meetings like ASGCT, we are exposed to the newest and most exciting ideas in gene therapy, which we hope they can bring back to the lab for implementation,” Dr. James said.
