Epilepsy Services
Diagnosis and Treatment Planning
Our Epilepsy Program experts have deep experience in diagnosing and treating children, teens and young adults with all types of seizures and epilepsy syndromes. We offer the following services to diagnose your child and plan their treatment.
First Seizure Clinic
We evaluate children who have had a seizure for the first time to learn more about the type of seizure, its cause and whether they may have epilepsy. It is important to determine if the seizure was caused (provoked) by a temporary problem like a concussion or high fever or is an epileptic seizure. Epilepsy is not the cause of seizures in up to half of children who visit our clinic.
- At your first visit, a neurology provider evaluates your child and talks with you about seizures.
- Your child may need a painless recording of the brain’s electrical activity, called an EEG. The EEG may happen that same day or during a return visit.
- Some children return to see a neurologist or epilepsy specialist.
Epilepsy Genetics
Our team of experts from different specialties is finding the changes in genes that cause many of the epilepsies seen in children. We do genetic testing to help diagnose epilepsy syndromes and pinpoint the cause of seizures. This helps us personalize care and may open the door to many more treatments. A diagnosis also provides connection with specific support and patient advocacy groups.
Our genetic counselors help families understand the chances of a genetic disorder happening in another pregnancy. They explain how other family members might be affected. Our experts also consult with healthcare providers about children at other centers.
Epilepsy Monitoring Unit (EMU)
We have a special area in our hospital for monitoring children’s brain activity, called the Epilepsy Monitoring Unit (EMU). We use EEG, a painless way to record the brain’s electrical activity. We also record your child by video camera to see and hear what happens when they have a seizure.
The recordings give us clues to their seizures. They help us diagnose your child, plan treatment and check how well medicine or other therapy is working.
Your child will stay in the hospital:
- 2 days if they are having EEG testing to help us understand more about their seizures
- 5 to 7 days if we are evaluating your child for surgery or other alternatives to medicine
A parent or caregiver will need to stay with your child the whole time. You know your child best and can help us tell when seizures are happening.
For more information, see Inpatient EEG Tests (PDF) (Spanish) (Russian) (Vietnamese)
Advanced neuroimaging
We use state-of-the-art devices that see inside your child’s brain (neuroimaging) to diagnose your child and recommend and plan the safest, most effective treatment.
Neuroimaging procedures make high-quality pictures of the brain’s structure and function. Your child may get 1 or more of these tests:
- MRI (magnetic resonance imaging) provides very detailed chemical and physical information about the brain. Seattle Children’s uses a 3.0 Tesla MRI scanner with 64 channels, which provides very fine detail of the brain and is better able to show where seizures are starting.
- PET (positron emission tomography) shows parts of the brain that use less energy. This can sometimes help us find where seizures start in your child’s brain.
- SPECT (single photon emission computed tomography) measures changes in brain blood flow during and between seizures. This can help us find where seizures start in your child’s brain.
- Functional brain MRI (fMRI) helps show if the brain area where seizures start is also used for important tasks like speaking. This helps guide surgery to be as safe as possible and avoid surgery if it is not the best treatment option. During the fMRI test, we will ask your child to do different tasks, such as tap their fingers together. We look at where brain signals start that tell your child to tap their fingers. This helps us to “map” their brain.
- Wada (WAH-dah) test determines which side of your child’s brain their language and memory abilities are located. Knowing this can prevent complications after surgery with your child’s speech and short-term and long-term memory. We give your child medicine to put 1 side of their brain to sleep. Then a neuropsychologist will ask your child to talk and remember simple objects. We test each side of the brain separately.
Advanced technology at Seattle Children’s lets us combine information from these images. This makes diagnosing your child’s epilepsy more accurate and improves their care.
Neuropsychological testing
This testing checks your child’s brain development and how the brain is linked to their behavior. We do many tests to check your child’s memory, attention, thinking, language skills, coordination, senses and personality. Read more about our Neuropsychology Evaluation (PDF) (Russian) (Spanish).
Intracranial EEG monitoring
If other tests don’t give enough information to decide if surgery is a good option and we want a more precise location of seizures, we may need to place electrodes inside your child’s skull (intracranial) on the surface of their brain to monitor for seizures. How we do this surgery depends on the number of electrodes and where we need to place them.
In more than 80% of intracranial EEGs, our neurosurgeons use ROSA robotic surgical tools that fit through tiny holes in the skull. This is called robot-guided stereo EEG or stereo electroencephalography (SEEG). In 20% of patients, neurosurgeons place the electrodes after removing part of the skull (craniotomy).
Intracranial monitoring may be needed if:
- Other tests do not show where your child’s seizures start
- The area identified as where seizures start is too large, and we need to narrow it down
- We need to know the location of seizure onset in relation to important brain functional areas
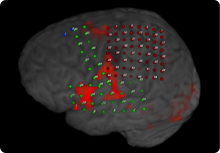 This image combines functional MRI with a grid of electrodes placed on the brain of a patient with epilepsy. The dots are electrodes, color-coded red (upper right), green (lower left) or blue (upper left) depending on the brain area they cover. The red patches show areas of the brain that are active during tasks related to language, movement and the senses.
This image combines functional MRI with a grid of electrodes placed on the brain of a patient with epilepsy. The dots are electrodes, color-coded red (upper right), green (lower left) or blue (upper left) depending on the brain area they cover. The red patches show areas of the brain that are active during tasks related to language, movement and the senses.Pictures from MRI scans guide surgeons as they work. A wand connected to the computerized guidance system tracks the location of tools. The image-guided system allows exact placement of electrodes and avoids disruption of critical brain areas.
Your child will stay in the hospital for 5 to 7 days for this type of monitoring. If they do not have seizures during this time, they will stay longer.
After testing, your child’s healthcare team will do another surgery to take off the electrodes and remove some brain tissue, if possible, to try to stop the seizures.
Epilepsy Treatment Options
There are many effective treatments to prevent or reduce seizures. We fully assess your child to decide the best treatment for them.
Medicines for seizures, including clinical trials
For almost all children with epilepsy, the first and most effective treatment is medicine. More than 30 medicines treat epilepsy. Different medicines are more effective for different types of seizures. These medicines are called anticonvulsants, antiepileptics or antiseizure medicines.
For children with epilepsy, medicine helps about 2 out of 3 stop having seizures. Most children and teens can control their seizures with just 1 kind of medicine. If seizures cannot be controlled by medicines alone, we call it intractable epilepsy.
Our work to identify genes that play a role in epilepsy has led to new therapies and specific protocols that help us personalize your child’s treatment. Our epilepsy team has access to many medicines, including some new options that are available to children who take part in research studies (clinical trials). These are especially relevant to children who have epilepsy syndromes or whose seizures are not controlled after trying 2 different medicines.
The goal of antiseizure medicine is to prevent seizures without causing major side effects. It may take a while to find the right medicine, schedule and amount. As needed, we test your child’s blood to make sure they have the right level of medicine to control their seizures.
The blood tests also check for signs of injury to your child’s body, such as to their liver. Medicines can have side effects and may affect your child’s emotions or thinking. If this happens to your child, your doctor may adjust the dose or change the medicine.
Nutrition therapy for epilepsy
If medicine does not control your child’s seizures, they may benefit from nutrition therapy — either the ketogenic diet or the modified Atkins diet. Diet therapy can lessen or stop seizures for some children. Usually, children still take medicine, but they can take less.
The nutrition team will help you decide if 1 of the diets is the right choice for your child. On both diets, children eat foods that are high in fats and low in carbohydrates. Our team helps to make sure your child is receiving nutrients they need to grow and keep a healthy weight. Children on these diets should always be under a doctor’s care.
Learn more:
- Ketogenic Diet and Your Child (PDF) (Arabic) (Spanish)
- Your Child’s Hospital Stay to Start the Ketogenic Diet (PDF) (Arabic) (Spanish)
Epilepsy Surgery Options
If neurosurgery is the right choice for your child, research shows it’s better to have the operation sooner rather than waiting. We do the following surgeries to help children with epilepsy.
Laser ablation surgery
For some children, laser ablation (LAY-zer ab-LAY-shun) surgery is an option with fewer side effects than traditional (open) surgery. This minimally invasive procedure uses light to heat and destroy unwanted cells. It offers the chance to live a seizure-free life for some kids who have run out of treatment options.
Seattle Children’s is among a handful of pediatric hospitals in the country — and the only 1 in our region — to offer laser ablation surgery for epilepsy.
Read more about laser ablation surgery for epilepsy.
Neuromodulation
Neuromodulation uses mild electrical pulses to change the way nerve cells communicate with each other. This can prevent or lessen seizures in children with epilepsy. Neuromodulation may be a good choice for your child if other treatments do not control their epilepsy. Neuromodulation reduces seizures but does not completely stop them.
During a surgery, a neurosurgeon places a device in your child’s body and connects it via tiny wires to specific areas of their brain or to the vagus nerve in the neck. Like a pacemaker, the device will not be visible after placement. A neurologist adjusts settings on the device for the best results for your child.
We offer 3 types of neuromodulation treatment for epilepsy:
- Responsive Neurostimulation System (RNS) (PDF) (Spanish) (Somali) (Vietnamese)
- Deep Brain Stimulation (DBS) (PDF) (Spanish) (Somali) (Vietnamese)
- Vagus Nerve Stimulator (VNS) (PDF) (Spanish) (Somali) (Ukrainian) (Vietnamese)
Our Neuromodulation Clinic brings together an expert team to diagnose and treat your child’s seizures. At our monthly clinic in Seattle, your child can get all their care in 1 setting.
Removing the seizure focus
If seizures start in a well-defined area of the brain (seizure focus), surgery to remove that area may stop or reduce your child’s seizures.
This is the most common type of surgery for epilepsy. It often helps children with abnormal brain tissue, such as:
- Mesial temporal sclerosis, which affects part of the brain underneath and behind the ears (temporal lobe)
- Cortical dysplasia, which affects the outer layer of the brain (cerebral cortex)
Removing brain tumors
Children with brain tumors that cause seizures can benefit from surgery to remove the tumor and a small amount of brain tissue around the tumor. Read more about how we treat brain tumors.
One cause of benign (noncancerous) brain tumors is tuberous sclerosis complex (TSC). Over 80% of patients with this rare genetic disease develop epilepsy.
Corpus callosotomy
The corpus callosum is a bundle of nerve fibers connecting the right and left sides of the brain. Neurosurgeons cut part or all of the corpus callosum to stop seizures from spreading from 1 half of the brain to the other.
This surgery helps children who have “drop-attack” seizures, where their muscles suddenly tighten and they fall down or collapse forward in a chair.
Hemispherotomy or hemispherectomy
These surgeries treat children with seizure focus areas throughout an entire half of the outer layer of the brain (cerebral cortex). The cortex controls many complex processes. Each half is called a hemisphere.
Your child’s neurosurgeon cuts and removes brain tissue to disconnect the affected half of the brain’s cortex from the other half. The goal is to prevent seizure activity from spreading throughout the brain.
The surgery is called functional hemispherotomy or hemispherectomy, depending on how it is done. This operation is shorter and causes fewer complications than older versions of the surgery, which removed half of the brain’s cortex.
Sometimes, a child’s brain function will move to the healthy side of the brain before or after surgery. But in most children, the surgery can have long-lasting serious effects, such as permanent weakness on 1 side.
Because of this, we only do this operation on children who:
- Have severe seizures that greatly limit their quality of life
- Are at high risk of death from seizures
- Are already weak on the affected side or we expect they will become weak because of a tumor or another brain problem
After surgery, most children need to stay in the hospital for physical therapy and occupational therapy to improve or manage weakness and their activities of daily living.
Contact Us
Schedule an appointment: 206-987-2016 or 844-935-3467 (toll free)
Meet the Seattle Children's Epilepsy Team.
Providers, see how to refer a patient.
Locations
- Seattle Children’s hospital campus: 206-987-2016 or 844-935-3467 (toll-free)
- Bellevue Clinic and Surgery Center: 206-987-2016 or 844-935-3467 (toll-free)
- Everett: 425-783-6200
- Federal Way: 206-987-2016 or 844-935-3467 (toll-free)
Telemedicine at Seattle Children’s
Your child’s first appointment in our clinic will be in person and take about 90 minutes. Later visits may be offered via telehealth (virtual). Learn more about telemedicine at Seattle Children’s.
Paying for Care
Learn about paying for care at Seattle Children’s, including insurance coverage, billing and financial assistance.
