Harrington Lab
The Harrington Lab is broadly focused on maternal-offspring immunity with a goal of translating our work to improve the health of the world’s women and children. Our main interests include (i) the role of maternal cells transmitted across the placenta and via breastmilk (known as maternal microchimerism) in shaping offspring immunity, (ii) determinants of differential immune responses in infants and children compared to adults and (iii) unique mucosal immunity present in the lactating breast and female genital tract. One shared feature across these interests is the challenge of investigating rare cells, which requires that we utilize cutting-edge approaches to study single cell biology.
We believe that science is always better (and more fun) within a strong community, and we collaborate widely across clinical and scientific domains, including many local labs at Seattle Children’s Research Institute, University of Washington, and the Fred Hutchinson Cancer Center, nationally and internationally.
The role of maternal cells in shaping offspring immunity
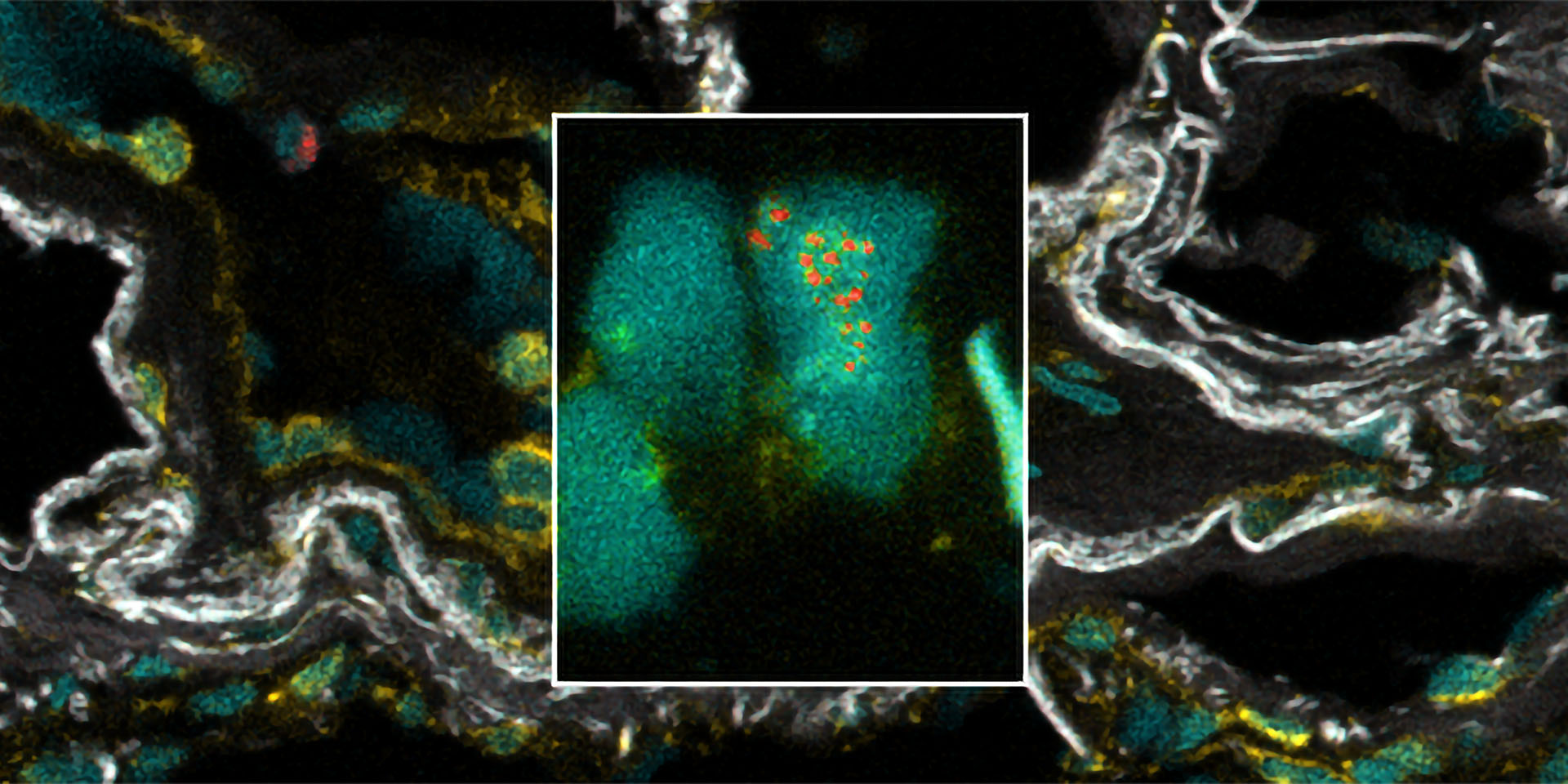
During pregnancy a mother transmits cells to her fetus, which can be detected at birth, during childhood, and even into adulthood, a phenomenon known as maternal microchimerism (MMc). Our work and the work of others has demonstrated that these cells are enriched for memory T cells, a type of immune cell which can persist for years to decades. Based on these observations, we hypothesize that in addition to short-lived protection provided by antibodies, mothers also gift their children with long-lived immune protection in the form of memory T cells. Supporting this hypothesis, we have found that infants with detectable MMc at birth are protected from symptomatic malaria, respiratory infection, and non-malarial fever, as well as develop improved responses to vaccination.
Our ongoing work seeks to demonstrate the mechanism behind these associations. We are investigating the antigen specificity of maternal T cells acquired by the fetus, with ongoing projects focused on P. falciparum (malaria), Mycobacterium, CMV, and vaccine-specific responses. In addition, we work to understand whether maternal cells can non-specifically shape offspring immune responses through accentuated innate immunity. This work relies on strong collaborations with the University of Washington Department of Obstetrics and Gynecology, as well as national and international collaborations.
Determinants of infant immune responses
It has long been recognized that infants and children display restricted immune responses to both pathogens and vaccines. This is particularly problematic in the case of liver-stage malaria vaccines, which to-date have demonstrated limited efficacy in African infants. Our ongoing collaborative work with the Minkah and Sodora labs investigates the factors that may restrict the development of hepatic tissue resident immunity in infants and children by seeking to characterize pediatric immune ontogeny in the human liver. This project was supported by an SCRI Team Science Ignition and relies on a strong collaboration with the Seattle Children’s Hospital Department of Pathology as well as University of Washington. In addition, we are interested in variable immune responses to vaccines in infants and adults more generally and recently published work investigating the quality of T cell responses to SARS2 mRNA vaccination in infants.
Non-invasive techniques to characterize human mucosal immunity
Our early work with the Jaspan lab identified that breastmilk exposure was a strong determinant of level of MMc in South African infants. This observation is consistent with literature from a variety of mammalian species demonstrating that nursing offspring can acquire a second graft of maternal cells from breastmilk. In order to characterize the immune cells present in human milk and to understand their ability to traffic to the infant, we recently characterized T cells present in breastmilk and demonstrated their response to SARS mRNA vaccination. In addition, we and others have demonstrated that breastmilk contains T cells specific to a variety of respiratory pathogens. These observations are now being extended by the work of the Armistead lab, our close collaborators. This project is supported by an SCRI Clinical-Research Synergy award and is in collaboration with Seattle Children’s Urgent Care with an ongoing project to enroll maternal-infant dyads with respiratory infections.
This work stimulated our interest in other techniques to non-invasively sample mucosal sites, and as a result, we recently developed a novel technique to characterize immune cells from the female genital tract using self-collected cervicovaginal disks. The female genital tract is key site of immune surveillance to colonizing microbes and immune response to pathogens, but it has been historically understudied due to challenges in sampling the space. We view this work as a form of scientific empowerment, as it is non-invasive and does not require a healthcare provider, thereby decreasing the barrier to participation in studies of the female genital tract. In ongoing work, we are assessing other approaches to sample the female genital tract non-invasively, as well as the ability to isolate pathogen and vaccine-specific T cells using these approaches. In addition, we are interested in using this approach to sample the immunity of the cervix during pregnancy, across the menopausal transition and following prophylactic and therapeutic vaccination.
Partnership Opportunities

Whitney Elizabeth Harrington, MD, PhD
Whitney Harrington, MD, PhD, is a member of the Center for Global Infectious Disease Research at Seattle Children’s Research Institute, an associate professor in the Department of Pediatrics, Division of Infectious Diseases, University of Washington, an adjunct associate professor in the Department of Global Health, University of Washington, and an affiliate investigator at Fred Hutchinson Cancer Center. Her research is supported by grants from NIH’s National Institute of Allergy and Infectious Diseases and Eunice Kennedy Shriver National Institute of Child Health and Human Development, the Swiss National Science Foundation, the Fondation Ernst & Lucie Schmidheiny, and the internal SCRI “Clinical-Research Synergy” and “Team Science Ignition” awards.
-

John Houck
Lab Manager
-

Yonghou Jiang
Research Scientist IV
-

Jacquelyn Weaver, MS
Student Helper
Seattle Children’s
- Dr. Heather Jaspan
- Dr. Blair Armistead
- Dr. Nana Minkah
- Dr. Lisa Frenkel
- Dr. Nina Derby (Sodora Lab)
- Dr. Janet Englund
- Dr. Gail Deutsch
- Dr. Jay Santos
University of Washington
- Dr. Alisa Kachikis (Dpt of OB/GYN)
- Dr. R. Swati Shree (Dpt of OB/GYN)
- Dr. Lucia Vojtech (Dpt of OB/GYN)
Fred Hutchinson Cancer Center
- Dr. Meghan Koch
- Dr. Martin Prlic
