Study Offers Good News on COVID-19 Immunity
1.7.2021 | Seattle Children's Press Team
 Pictured from left to right: Yu Chen, Malika Hale and Christopher Thouvenel of the Rawlings lab at Seattle Children’s Research Institute.
Pictured from left to right: Yu Chen, Malika Hale and Christopher Thouvenel of the Rawlings lab at Seattle Children’s Research Institute.
For close to a decade the labs of Dr. David Rawlings at Seattle Children’s Research Institute and Dr. Marion Pepper at the University of Washington have collaborated on a project studying the immune response in malaria infections.
As the COVID-19 pandemic gripped the U.S., they turned their expertise and the techniques pioneered for malaria to a new line of inquiry: Did mild infection from the new coronavirus stimulate the immune system to generate antibodies that would offer future protection from the virus? And if so, could they engineer those neutralizing antibodies in the lab to develop potent new therapeutic options?
Rawlings, the director of the Center for Immunity and Immunotherapies at Seattle Children’s and a professor of pediatrics at UW, discusses their encouraging findings now published in Cell. Learn why he says their research is good news for efforts to control COVID-19 and what’s next for his lab.
Q: How did you translate your work in malaria to the current pandemic?
A: One of the main goals of our collaboration with Marion’s lab has been to identify the memory B cells our immune system produces in response to an infection. Memory B cells recognize specific pathogens, like the novel coronavirus, and produce large amounts of antibodies to fight off future infections. Much of our work in this area has focused on isolating memory B cells in malaria, a deadly disease that infects over 200 million each year to develop a better vaccine and more effective therapies.
Marion has pioneered a method that allows us to look at the surface of a memory B cell and see what pathogen it recognizes. Once they isolate these rare immune cells using isolation of single cells by flow cytometry cell sorting, scientist Christopher Thouvenel in my lab uses cutting-edge molecular biology techniques to identify the antibody that each B cell would make. By analyzing the antibodies, we can say a lot about the immune response to the malaria parasite, virus, or other pathogen.
The real power, though, comes from taking the DNA sequence from each memory B cell to make lab-engineered antibodies called monoclonal antibodies, or mAbs. Using this approach, we’re able to make a whole series of mAbs to malaria proteins that we think are potentially protective.
We had optimized this approach over the last five to six years studying malaria, and so when COVID-19 appeared, we had the opportunity to apply the highly efficient method we had in place to study the immune response to a COVID-19 infection.
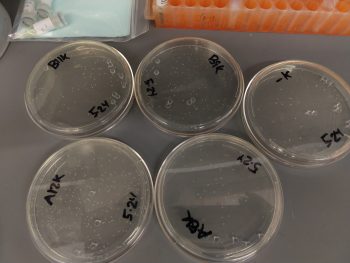
Creating monoclonal antibodies is a multi-step process that requires a variety of molecular biology techniques. This photo shows plates of bacteria that have been engineered to produce the DNA instructions needed for making antibodies.
Q: What did this research confirm about the long-term immune response to the new coronavirus?
A: This paper looks at the two arms of the immune system that are the most important to an immune response, the T cells and B cells. The UW team looked for T cells and B cells specific to the novel coronavirus in samples provided from 14 study volunteers who had recovered from mild COVID-19 symptoms. The samples were collected at about one month and three months after infection.
Encouragingly, they found that recovered individuals developed the full-range of virus-specific immune cells and antibodies and that these persisted for at least three months. Their analysis also revealed that memory B cells increased over time.
When we looked at the antibodies we had expressed from the memory B cells, we found that these antibodies recognized the surface protein found in the new coronavirus, proving that the B cell was in fact virus-specific. The antibodies were also capable of protecting from viral infection, or what we call neutralizing antibodies.
Neutralizing antibodies bind to the surface of a virus in way that blocks the virus from infecting a healthy cell. One of the ways we determine whether an antibody is neutralizing is to see if it can block a real viral infection in the lab. Here, the teams partnered with the lab of Dr. Michael Gale who used the Biocontainment Safety Level 3 Laboratory at UW, which is necessary to do experiments with the new coronavirus.
The results are exciting because of the 15 mAbs that were tested, about 40-50% were highly active neutralizing antibodies. We also showed that neutralizing antibodies increased from the first sample collection to the second, indicating that as the memory immune responses matured, it also became more robust. Altogether, our research offers compelling evidence that mild COVID-19 leads to a persistent memory immune response and antiviral immunity that could potentially offer protection from reinfection.
Q: Why are the antibodies your lab expressed as part of this research important to ongoing drug development efforts?
A: The ideal mAb therapy to treat COVID-19 would have a mixture of two to three highly neutralizing antibodies that recognize distinct parts of the virus and that form strong bonds with the virus. This research produced several strong candidates and we hope to partner with companies that can potentially bring them to clinical use.
Q: What questions remain about immunity to the new coronavirus?
A: These are emerging data that show a memory immune response to COVID-19, but no one knows how long its duration will be. We know that the types of memory cells we’re seeing can last a long time in other viral responses, so there’s reason to believe it may be long-lasting.
The importance of long-lasting immunity also applies to the vaccines now in use. We don’t yet know the long-term protection of these vaccines or whether they produce the same types of neutralizing antibodies we found in this study.
Q: What’s next for your lab?
A: We will continue to collect samples from our study volunteers and data as part of this study over the next year.
We’re also looking at ways we might enhance the structure of our mAbs using a technique we’ve developed from our malaria research. We’ve found that different formats of the antibody can produce different functional capabilities and binding abilities. With this technique, we think we can make them bind up to 10 times better. All of this is important to understand the best antibodies to use clinically, possible also allowing for activity at lower doses and driving more effective viral killing.
Another exciting project we hope to get underway involves testing our neutralizing antibodies in the cells that line the lungs. The COVID-19 infection targets these airway epithelial cells and it has yet to be tested whether neutralizing antibodies can block the virus in that environment. Dr. Jason Debley has developed a way to grow human airway epithelial cells in his lab at Seattle Children’s and partnering with him on this work could yield valuable insight into how our immune system attacks COVID-19 infections in the lungs.
Dr. Yu Chen and UW-PhD student, Malika Hale, also contributed to this research from the Rawlings lab. Rawlings received a Seattle Children’s Research Integration Hub COVID-19 Award to support this research. It is one of more than 50 research studies underway at Seattle Children’s to understand, detect, treat and prevent the novel coronavirus in children and families.