Powell Lab
Research in the Powell Lab uses molecular and physiologic measures of circadian rhythms to define the roles of the circadian clock and time in human airways and lung diseases. We conduct mechanistic research using primary airway epithelial cells with linked patient characterization in order to link the molecular clock to clinically-oriented outcomes and measures. We focus on how circadian machinery intersects with mechanisms driving viral responses linked to asthma exacerbations, airway remodeling and disease outcomes.
We also explore how the clock in the airway epithelium functions in multiple airway diseases, such as pediatric obstructive sleep apnea (OSA), pediatric asthma, and viral infections e.g. croup. Leveraging an understanding of chronobiology in human disease, we aim to answer not only “what and why” of disease pathogenesis and treatment, but also “when.”
Circadian Clock in Human Airway Epithelia
 Many diseases, including asthma, croup, viral infections and allergic rhinitis, demonstrate a diurnal, or time of day, difference in their presentation and severity.
Many diseases, including asthma, croup, viral infections and allergic rhinitis, demonstrate a diurnal, or time of day, difference in their presentation and severity.
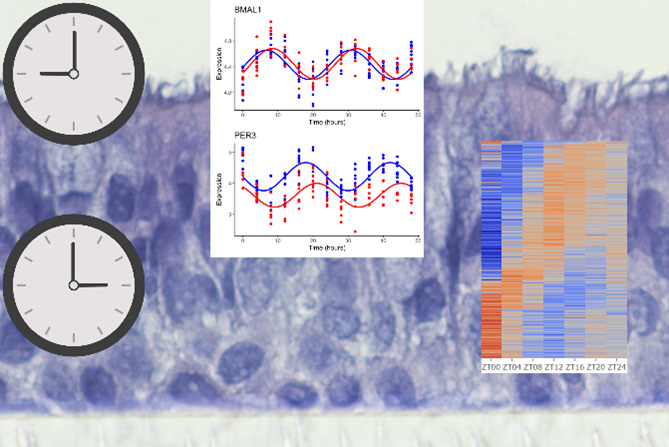
Mouse models have identified the molecular circadian machinery as having an integral role in regulating immune and inflammatory responses. However, our understanding of how molecular circadian machinery intersects with human disease presentations remains limited due to the difficulty in obtaining repeated functional and molecular tasks in humans.
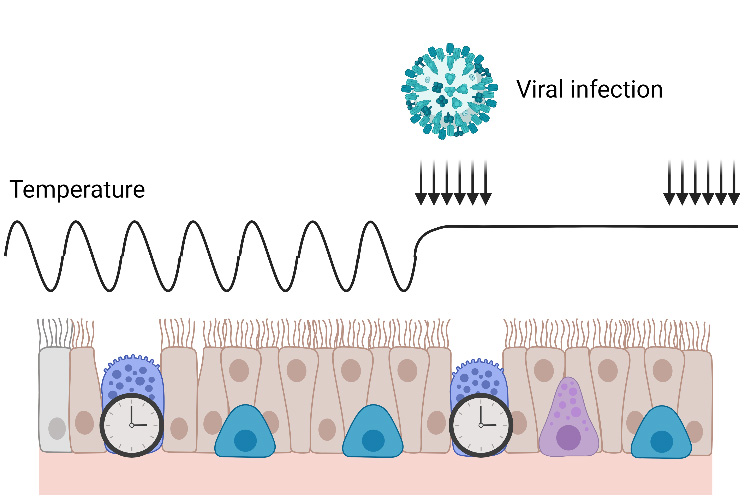
We use an ex vivo organotypic model of the human airway epithelium to conduct mechanistic studies of circadian regulation in viral infections and with direct disease relevance. Using temperature-cycled incubators we synchronize endogenous circadian rhythms by mimicking in vivo temperature rhythms to introduce the element of time of day to our experiments. We are characterizing molecular rhythms in patient-derived primary airway epithelial cells in order to link dysregulation of molecular pathways back to clinical characteristics.
This work will help to further understand diseases like asthma, pediatric OSA, allergic diseases and viral infections.
Airway Epithelial Responses in Airway Diseases
 Asthma and Pediatric OSA are common airway disorders in children. Asthma, pediatric OSA, and allergic rhinitis are often comorbid in children suggesting a common underlying pathogenesis at the level of the airway epithelium. While the role of the airway epithelium has been extensively characterized in allergic disease and in pediatric asthma, the role of the airway epithelium in the pathogenesis of pediatric OSA remains under studied.
Asthma and Pediatric OSA are common airway disorders in children. Asthma, pediatric OSA, and allergic rhinitis are often comorbid in children suggesting a common underlying pathogenesis at the level of the airway epithelium. While the role of the airway epithelium has been extensively characterized in allergic disease and in pediatric asthma, the role of the airway epithelium in the pathogenesis of pediatric OSA remains under studied.
Current treatment of pediatric OSA is primarily surgical (adenotonsillectomy) or mechanical (continuous positive airway pressure, CPAP) with limited medical interventions available.
Our research investigates how airway epithelial immune and inflammatory pathways may play a role in the pathogenesis and presentation of pediatric OSA. In doing so we aim to identify novel potential therapeutic options to allow for a more personalized and directed approach to the treatment of pediatric OSA.

Weston Thomas Powell, MD, PhD
Dr. Powell received an MD and PhD from UC Davis. He completed Pediatric Residency, Sleep, and Pulmonary Fellowship at UW and Seattle Children’s Hospital. He joined the division of Pediatric Pulmonary and Sleep Medicine at UW and Seattle Children’s Hospital in 2023.
-
Nina Daluz
Undergraduate Researcher
-

Ana Jahn
Research Associate
-
Maria Kang
Undergraduate Researcher
-

Maddie Ohm
Research Scientist I
-

Jade Turner
Clinical Research Coordinator
