Debley Lab
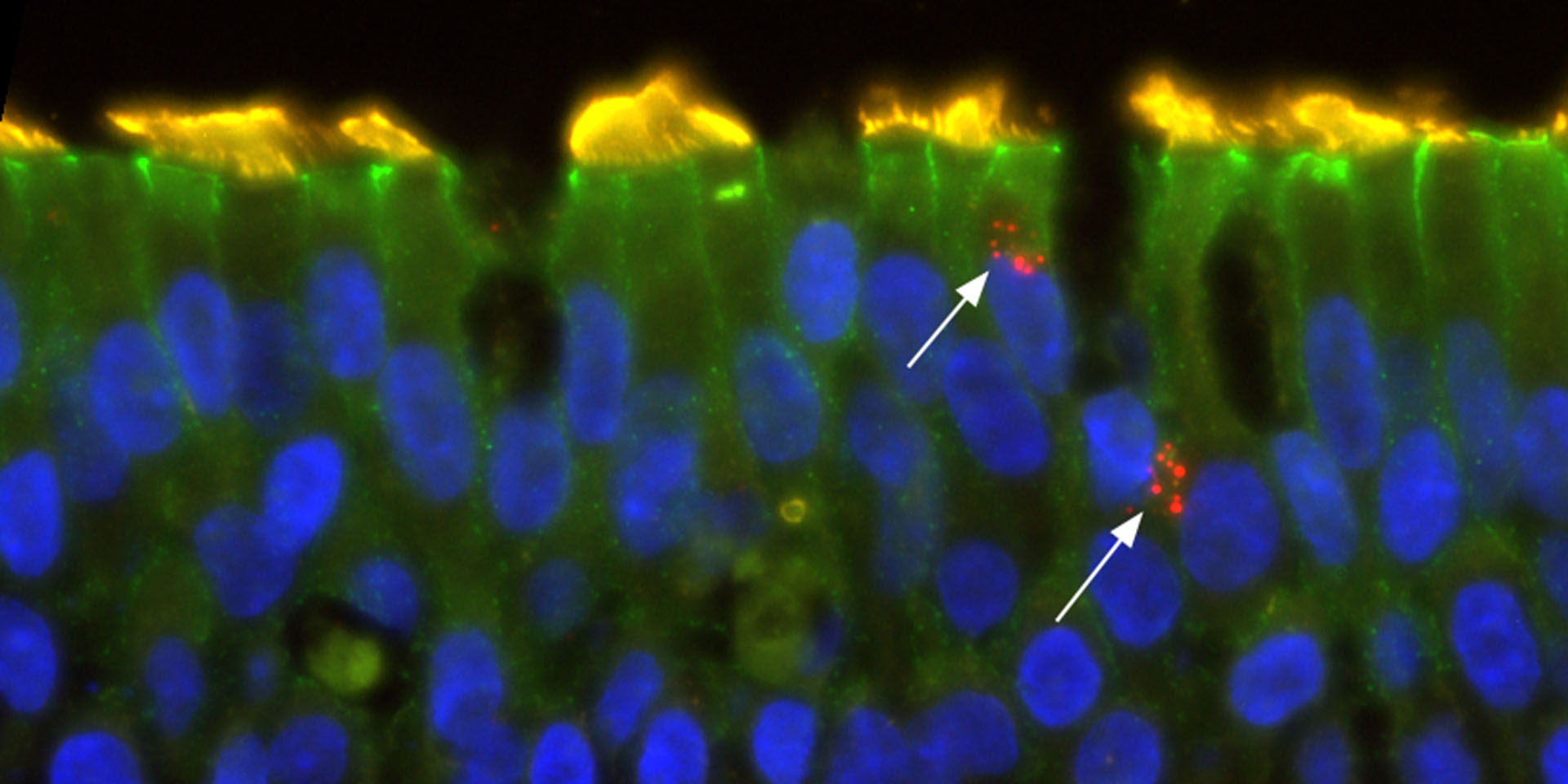
Investigating epithelial responses to viruses and signaling pathways regulating airway remodeling in childhood asthma.
The Debley Lab conducts an array of patient-oriented mechanistic research using primary bronchial epithelial cells from carefully phenotyped, endotyped, and genotyped children with asthma and healthy children to investigate innate immune responses to respiratory viruses (e.g. human rhinovirus, RSV) and mechanisms underlying viral-triggered asthma exacerbations and airway remodeling.
Research conducted in the Debley Lab seeks to investigate roles of airway epithelial cells in the pathobiology of asthma and other airway disease. Primary focus areas include:
- Improve understanding of the heterogeneity of airway epithelial interferon responses to respiratory viruses in asthmatic and healthy children and how deficient or excessive interferon responses impact the risk of asthma exacerbations, airway remodeling responses and lung function.
- Investigate airway epithelial cell signaling pathways that regulate responses by immune cells (e.g. mast cells, eosinophils, T cells) and neighboring stromal cells (e.g. fibroblasts/smooth muscle cells) and how such pathways are dysregulated in asthma leading to airway remodeling and lung function abnormalities in epithelial cell donors.
Dr. Debley’s research program has obtained primary bronchial and nasal epithelial cells from children with and without asthma who are undergoing elective surgical procedures at Seattle Children’s Hospital since 2007. This infrastructure is a unique resource in the U.S., providing a steady source of primary bronchial airway epithelial cells from carefully characterized children to conduct mechanistic investigations (stratified by donor clinical characteristics such as lung function, exacerbation history, endotype and disease severity) to better understand the role of the epithelium in childhood asthma and responses to viral infection in health and disease.
Model systems used by the Debley Lab provide an ideal platform to test disease mechanisms, improve understanding of innate immune responses at the respiratory mucosal surface as well as to screen potential therapeutics in human cells from carefully clinically characterized, endotyped and genotyped children.
Latest News and Publications
- March 29, 2023 Type 2 inflammation reduces SARS-CoV-2 replication in the airway epithelium in allergic asthma through functional alteration of ciliated epithelial cells
- March 13, 2023 Sputum periostin is a biomarker of type 2 inflammation but not airway dysfunction in asthma
- October 9, 2022 Temperature synchronisation of circadian rhythms in primary human airway epithelial cells from children
See all publications.
Meet the Team

Jason Scott Debley, MD, MPH
Dr. Jason Debley’s research has spanned clinical, epidemiologic, basic and mechanistic patient-oriented translational asthma research. His work over the past two decades has concentrated on investigation of the role of the airway epithelium in asthma pathobiology, with focus areas including study of innate immune responses of airway epithelial cells to respiratory viruses and aberrant epithelial regulation of airway remodeling responses. He built a translational research program wherein primary bronchial epithelial cells are obtained from asthmatic and healthy children undergoing elective surgical procedures at Seattle Children’s Hospital. This infrastructure is a unique resource in the U.S., providing a steady source of primary bronchial airway epithelial cells from carefully characterized children with and without asthma that are used to conduct mechanistic research. A highly innovative aspect of his program is that ex vivo experiments are conducted using primary airway epithelial cells from donors who are genotyped for polymorphisms of interest and stratified by clinical characteristics of donors (e.g. T2 vs. non-T2 endotype based on biomarker signatures, exacerbations, lung function), and donors are prospectively followed to track incident exacerbations and lung function change over time. This allows for investigation of disease mechanisms using data linking ex vivo mechanistic experiments to asthma endotype/phenotype, donor genotype, and longitudinal donor clinical outcomes. Dr. Debley also serves as director of the Center for Respiratory Biology and Therapeutics (CRBT) at Seattle Children’s Research Institute.
 Patricia Andrea dela Cruz, MD, PhD
Patricia Andrea dela Cruz, MD, PhD
Allergy Fellow
 Camille Gates, BS
Camille Gates, BS
Lab Technician II
 Weston Thomas Powell, MD, PhD
Weston Thomas Powell, MD, PhD
Assistant Professor
 Lucille Rich, BS
Lucille Rich, BS
Research Scientist I
 Nyssa Becker Samanas, PhD
Nyssa Becker Samanas, PhD
Research Scientist IV
 Elizabeth Vanderwall, BS
Elizabeth Vanderwall, BS
Research Scientist I
 Maria White, BA
Maria White, BA
Clinical Research Coordinator II
 Sathi Wijeyesinghe, MD, PhD
Sathi Wijeyesinghe, MD, PhD
Allergy Fellow
