Early Recognition of Common Pediatric Hand Problems: A Q&A With Dr. Suzanne Steinman
February 3, 2021
Dr. Nicolas Fernandez is a pediatric urologist. He joined Seattle Children’s in 2020. An artist also, he illustrated the images for this article.
Q: When does buried penis in an obese child require surgery?
 Dr. Fernandez: This is a very interesting topic. Genital, and more specifically penile, appearance is very subjective and varies from culture to culture. There are three different types of buried penis, also known as hidden penis.
Dr. Fernandez: This is a very interesting topic. Genital, and more specifically penile, appearance is very subjective and varies from culture to culture. There are three different types of buried penis, also known as hidden penis.
- Secondary to obesity
- Secondary to poor penile pubic and penoscrotal fixation of the skin
- Secondary to prior penile surgery that creates a trapped penis
Surgical intervention is rarely done for patients with a buried penis that is secondary to obesity in the pediatric population. The first thing that it is important to highlight is that the clinician needs to establish whether the penile size is normal or not. In most cases where obesity is the cause of buried penis, the penile length will be normal. When counseling families, it is important to explain this and to consider the expectations of the patient and the family.
Another important topic to cover with families and patients is the natural history of penile growth. Boys typically have an initial growth of their penis during the first three months of life as a result of increased testosterone production by Leydig cells. This is called the mini-puberty phase. After that, the penis does not grow significantly until puberty starts. It is critically important to guide patients and families to focus on managing the child’s obesity/weight and giving time for the penis to grow.
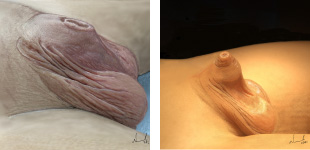 Buried penis with indication for surgery on non-obese patients. Left: megaprepuce buried penis. Right: penoscrotal webbing and buried penis.
Buried penis with indication for surgery on non-obese patients. Left: megaprepuce buried penis. Right: penoscrotal webbing and buried penis.The appearance of a buried penis usually improves with weight loss in the obese child and giving it time to grow around puberty. Buried penis is a situation that rarely creates any voiding issues to the patient.
In cases where buried penis is secondary to poor penopubic and penoscrotal fixation of the skin, a surgical intervention might be considered. Surgery is also necessary to correct prior penile surgery that creates a trapped penis, and this additional second surgery can be expected to be more complicated.
Q: In the case where a newborn has scrotal webs, should I hold off on circumcision?
Dr. Fernandez: Neonatal circumcision has the great benefit of avoiding general anesthesia. Having had the experience of working in other countries around the world where neonatal circumcisions are not a regular practice has given me the opportunity understand the benefits but also the downsides of this procedure. I believe that the decision to perform a neonatal circumcision should be based on the anatomy of the penis. If the anatomy is not favorable, all neonatal circumcision should be avoided due to the risk of redundant foreskin and trapped penis and penoscrotal webbing after the procedure. This is in fact a common complaint in our clinics and a leading cause for surgical interventions in the pediatric population. If there is a question about mild webbing, I would suggest avoiding a neonatal circumcision and refer the patient to Pediatric Urology. Even mild penoscrotal webbing cases where a neonatal circumcision is done might have a high likelihood of requiring a surgical intervention for reconstruction, in addition to exposure to an anesthetic and the challenge of not having enough skin to be reconstructed.
Q: What do you recommend for patients with suspected meatal stenosis?
Dr. Fernandez: The condition of meatal stenosis is, from my personal perspective, quite uncommon in uncircumcised patients. I have identified that most of the referrals where there is a question about meatal stenosis are mostly due to irritative low urinary tract symptoms but rarely due to clearly obstructive symptoms. Meatal stenosis is more frequent in circumcised boys that present with deflected urinary stream that is straight and points upwards. The appearance of the urethral meatus does not correlate with the quality of the stream or how compliant the urethral meatus might be.
When evaluating patients, they usually have associated constipation that creates dysuria and pruritus (itchiness) at the tip of the penis. Pediatric patients rarely have had instrumentation, which is a common cause of meatal stenosis. The cases where I have identified meatal stenosis are associated with lichen sclerosis (or balanitis xerotica obliterans, BXO).
Q: How long should a patient be treated with antibiotics for uncomplicated UTI, and does it differ for boys and girls? Do teen boys with UTI need longer treatment than teen girls?
Dr. Fernandez: Our Seattle Children’s algorithm for UTI recommends:
- Non-toilet-trained children: 10 days
- Toilet-trained: 7 days
- Teens with cystitis: 3 days
Management of UTI should not be changed based on sex. It’s important to emphasize that a teenage boy should not get a UTI infection. If you document an infection in this population, please refer the patient to Urology as part of your management.
If you look at in vitro studies, you can see that within 12 hours of oral antibiotics you can sterilize the urine and potentially treat the infection. The reason for establishing the time frames above is to clinically treat the infection in order to reduce the chances of recurrence or of having a partially treated infection. One thing that we do not recommend is getting post-treatment urine cultures if the symptoms have improved.
Q: What is Seattle Children’s Urology seeing via telehealth, and what needs to be in person?
Dr. Fernandez: Telehealth has been an incredible addition to our practice, and we anticipate it will become a regular tool even after the pandemic that will improve patient care and efficiency. We currently are using telehealth mostly for follow-up visits. For new visits, we have been seeing as in-person all referrals that suggest conditions such as phimosis, hypospadias, buried penis, labial adhesions, undescended testicles and other conditions requiring in-person assessment. We do have a dedicated multidisciplinary Stone Clinic that is exclusively telehealth. In the future, I believe that many cases of hydronephrosis, vesicoureteral reflux and other similar conditions can easily be seen via telehealth.
Resources
- Buried penis: patient information flyer (Spanish)
- Resources for providers on Urology’s Refer a Patient page
- Antenatal Hydronephrosis and Undescended Testes: A Q&A With Dr. Paul Merguerian
- Enuresis/incontinence (daytime and nighttime)
- Hydronephrosis: Algorithm
- Phimosis: Information for PCPs and algorithm
- Undescended testes
- UTI: Information for PCPs and algorithm
- Varicocele: Algorithm
- Vesicoureteral reflux (VUR)