Aerodigestive Program
Contact the Aerodigestive Program
What is the Aerodigestive Program?
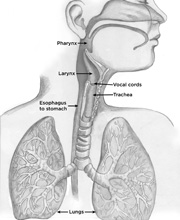 At Seattle Children’s Aerodigestive Program, we treat children, from birth to age 21, who have complex airway, breathing and swallowing problems as part of our larger Airway and Esophageal Center. The word “aerodigestive” combines “aero,” which means “air,” and “digestive.” In this program, we treat airway and digestive tract issues that are closely tied together. These problems can involve a child’s:
At Seattle Children’s Aerodigestive Program, we treat children, from birth to age 21, who have complex airway, breathing and swallowing problems as part of our larger Airway and Esophageal Center. The word “aerodigestive” combines “aero,” which means “air,” and “digestive.” In this program, we treat airway and digestive tract issues that are closely tied together. These problems can involve a child’s:
- Mouth and throat (pharynx)
- Voice box (larynx)
- Windpipe (trachea)
- Lungs
- Food pipe (esophagus)
- Stomach
-
Interdisciplinary team
We see problems that involve a child’s digestive, airway and respiratory systems. The structures and functions of these systems in the body are all connected. We believe that the best care starts with a coordinated, interdisciplinary team. “Interdisciplinary” means that when we see patients, we communicate with each other and recommend next steps based on input from all team members. The Aerodigestive Program team includes the following specialists:
- Otolaryngologist (ear, nose and throat experts)
- Pulmonologist (lung experts)
- (experts in the digestive tract)
- Nutritionist (registered dietitians)
- Speech and language pathologist (experts in evaluating feeding and swallowing)
If your child needs to be seen by additional specialists, we will coordinate those services on the same day as your initial appointment if possible.
-
We treat health conditions that are linked and complex
The children we see in the Aerodigestive Program have been referred to us because they have several health issues that are linked with each other. To solve one problem, the other problems must be treated as well.
These linked health issues happen because the tube-like parts of our body that we use for breathing and swallowing share physical space. There is an opening in the voice box (larynx) between the vocal cords. This opening connects to the windpipe (trachea), which connects to the lungs. This area is known as the body’s airway. Behind the trachea is the opening to the food tube (esophagus), which leads to the stomach and intestines. When everything is working well, food and air take different paths:
- Food travels from the mouth to the throat to the esophagus to the stomach.
- Air travels from the mouth to the throat to the larynx to the trachea to the lungs.
Each child we treat has a unique mix of digestive, respiratory and/or pulmonary issues causing them distress. For example, we might see a child who has severe reflux (where food and stomach acid back up into the esophagus) and has recurring pneumonia (a lung infection) as a result of aspirating (breathing in) their reflux. Through talking to you and your child and through diagnostic tests, we might learn that:
- Stomach acid from the severe reflux is causing damage to your child’s swallowing reflexes.
- Swallowing trouble is causing food or stomach content to accidentally get into the lungs (aspiration).
- More frequent aspiration is leading to more bouts of pneumonia.
You’ve probably had the experience of food “going down the wrong pipe.” This can happen in children when they have trouble swallowing (called dysphagia). Instead of food staying in the esophagus, some of it takes a detour through the larynx and into the lungs (aspiration). Many of the children we see in the Aerodigestive Program have dysphagia and aspiration, as well as frequent lung infections from chronic aspiration.
There are many aerodigestive problems other than dysphagia and aspiration that we manage. Some children we see have conditions that develop because they have a narrowing of the airway (subglottic stenosis) and might need reconstructive surgery. Some children are born with subglottic stenosis, and some develop it from having a breathing tube (ventilator) for a long time. Other children we see are having trouble with the transition from breathing through a tracheotomy tube to breathing on their own, and we have been asked to investigate the causes.
Because our mission is to treat complex, linked aerodigestive conditions, we don’t have a “typical” patient. Most of our patients have been referred to us by other specialists because of the complex nature of their conditions.
After identifying the problems and how they are connected, we create a care plan that spans your child’s respiratory, digestive and pulmonary systems. The care plan includes the caregivers who are experts in those systems.
How will the Aerodigestive Program meet my needs?
-
One clinic visit, many experts
If your child is referred to the Aerodigestive Program, you will first visit our clinic at Seattle Children’s Bellevue Clinic and Surgery Center. A team of experts will ask you and your child questions about their medical history. They will also examine your child, perform or schedule necessary tests, and answer questions. Our dedicated coordinators will assist you with all scheduling needs.
The length of your visit depends on your family’s needs, the number of providers your child needs to see and the tests your child may need. Most visits last 3 to 5 hours.
During your initial visit, you will meet with our primary team of experts who will work together throughout your child’s clinic visit to develop a patient-focused plan. At the end of the visit, a nurse or other team member will meet with you to review the comprehensive care plan and recommendations. One benefit provided by the Aerodigestive Program is an interdisciplinary review of all care plans by the entire team included in your child’s visit. If any changes are recommended after this discussion, families will be contacted by a team representative.
-
Coordinated same-day testing at clinic visit
Your child may receive some or all of these tests during their visit:
- Hearing test
- X-ray of neck, chest or abdomen
- Pulmonary function tests (PFTS [PDF]). Breathing exercises to better capture a child’s lung volumes. These tests are only given to children ages 5 and up.
- Flexible fiber-optic laryngoscopy [PDF]. An otolaryngologist will insert a small flexible telescope through the nose to evaluate the throat and voice box. This is brief and is done while the child is awake.
- Fiber-optic Endoscopic Evaluation of Swallowing (FEES [PDF]). An otolaryngologist will insert a thin flexible telescope into the nose while the child is feeding. This lets us look at their throat while they are swallowing.
- Videofluoroscopic Swallowing Study (VFSS [PDF]). A VFSS is a test to look at how your child swallows foods and liquids. We make an X-ray “movie” of the mouth and throat while they are drinking and eating to determine if anything travels into their airway instead of their food tube (esophagus).
- Lab tests. We may need to draw blood to determine important information about your child’s health. The team will let you know if this is required.
The results from these tests help the Aerodigestive Program create their care plan. The team may need more information after the clinic visit. If this is the case, our coordinator will assist you with scheduling. If your child requires one or more endoscopies under anesthesia, these will be scheduled at a later time.
-
Coordinated endoscopies
After your Aerodigestive clinic visit, your child may need further testing such as one or more endoscopies. An endoscopy is a test that lets the doctor look inside your child’s body with a small camera through a small opening such as the mouth. Your child will be given general anesthesia or sedation during an endoscopy so they will be comfortable. Our team has many years of experience performing endoscopies on children. We take care to ensure each procedure is safe and as comfortable as possible.
Endoscopies are done at the main hospital campus in Seattle. We coordinate these tests so that they can be done in one visit to the operating room. This means your child can get all tests performed in about 1 to 2 hours. The endoscopies that we perform include:
- Esophagogastroduodenoscopy (EGD). A gastroenterologist uses a flexible scope to look at the esophagus, stomach and upper gastrointestinal (GI) tract. The doctor often obtains samples of the lining of these areas as well. Learn more about this type of endoscopy (PDF).
- Flexible bronchoscopy and bronchoalveolar lavage (BAL). A pulmonologist uses a small flexible scope to look at the movement of the upper and lower airways while your child is lightly sedated and breathing on their own. The doctor also performs a washing of the lungs, which gives them cell samples that they can study. Learn more about this type of bronchoscopy (PDF).
- Microdirect laryngoscopy and bronchoscopy (MDLB). An otolaryngologist uses a very small, rigid telescope, which is passed through the mouth to get an enlarged view of the voice box and windpipe.
The doctors who perform the endoscopies will meet with you and your child to give you the results, schedule a follow-up visit and discuss the next steps.
Examples of the types of next steps we might recommend are:
- Sleep studies
- Imaging such as chest CT (computed tomography) scans or head MRI (magnetic resonance imaging) scans
- Repeats of certain tests after treatments have been prescribed to see if a child’s condition has improved
- Surgery
-
Talking to each other is built into our mission
We see how frustrating it is for parents who have a child with a complex aerodigestive condition that requires care by multiple doctors. Our program is not a group of individual doctors focused on individual symptoms. Our goal is to treat the whole child and to improve health problems that are linked to each other. That is why communicating with each other is a priority. It is also important to us to communicate well with you and the physician who referred you to the program.
After all tests and endoscopies have been completed, team members meet together in person, discuss what we have learned and agree on the next steps. We believe that collaborating is crucial to providing the best possible treatment for our patients. Once we agree on a diagnosis, we present our findings and recommendations – together as a team – to patients and their families.
For patients’ families, we have an online patient portal set up for direct communication with the team. We are here to answer questions. We want to keep the conversation going.
Who’s on the team?
Aerodigestive Program caregivers have special training not only in their fields, but also in the unique needs of children and adolescents.
Teams
Otolaryngology
-
Sparrow Helland, RN
Pulmonary
-
Debbie Morgan, RRT, RPFT
-
Brad Reece, RRT, CPFT
Gastroenterology
Speech and language pathology
-
Alexander Berg, MS, CCC-SLP
-

Kim DeMarre, MS, CCC-SLP
-

Amy Faherty, MS, CCC-SLP
-
Emily Zezas, MA, CCC-SLP
Contact Us
If you have a referral or would like a second opinion, or for more information about the Aerodigestive Program, call 206-987-6587.
Schedule an appointment with the Aerodigestive Program
- To make an appointment with Seattle Children’s Aerodigestive Program, you need a referral from your primary care doctor or specialist. If you already have a referral, call our scheduler at 206-987-6587 to make an appointment.
- See our Insurance Services page for answers to your questions about insurance coverage.
Telemedicine at Seattle Children’s
Your child’s first appointment in our clinic will be in person and take about 90 minutes. Later visits may be offered via telehealth (virtual). Learn more about telemedicine at Seattle Children’s.
Make a referral
If you are a referring physician and would like to talk to a member of the Aerodigestive team about a patient, call the Otolaryngology nurse line at 206-987-2105. Even if you are unsure about whether your patient should be seen by us, we want to help you with any questions you might have.
What should I bring to my child’s appointment?
- Books, toys and snacks for your child
- Your child’s clinic notes or reports about operations done outside of Seattle Children’s
- Your child’s imaging or study results done outside of Seattle Children’s, like X-rays, swallow studies, sleep studies, growth charts and reports of blood work or other tests
- Your child’s medicines and medical equipment
- Forms that providers need to sign, like school forms
- 3-day food diary, if your child is eating by mouth
- Cup or bottle your child prefers
Resources for Patients and Families
Paying for Care
Learn about paying for care at Seattle Children’s, including insurance coverage, billing and financial assistance.
Access Additional Resources
Get resources for patients and families, including information on food, housing, transportation, financial assistance, mental health and more.
















