Airway Cells in Children With Allergic Asthma Protect Against COVID-19 Infection
 May 31, 2023 – Researchers in Seattle Children’s Research Institute's Center for Respiratory Biology and Therapeutics (CRBT) and collaborators discovered why children with allergic asthma may have reduced susceptibility to COVID-19 — despite well-known susceptibilities to other respiratory viral infections — and an important mechanism by which allergic inflammation diminishes SARS-CoV-2 (the virus that causes COVID-19) infection. The findings were recently published in the Journal of Allergy and Clinical Immunology.
May 31, 2023 – Researchers in Seattle Children’s Research Institute's Center for Respiratory Biology and Therapeutics (CRBT) and collaborators discovered why children with allergic asthma may have reduced susceptibility to COVID-19 — despite well-known susceptibilities to other respiratory viral infections — and an important mechanism by which allergic inflammation diminishes SARS-CoV-2 (the virus that causes COVID-19) infection. The findings were recently published in the Journal of Allergy and Clinical Immunology.
Allergic diseases such as asthma are characterized by type-2 inflammation in the airways. This type of inflammation is an immune response to an allergen. The majority of people with asthma have type-2 inflammation.
The research team, including colleagues at the Benaroya Research Institute (BRI), University of Washington School of Medicine, National Institute of Allergy and Infectious Diseases and University of Wisconsin, looked at mechanisms by which type-2 inflammation in the airway surprisingly protects against SARS-CoV-2 in children.
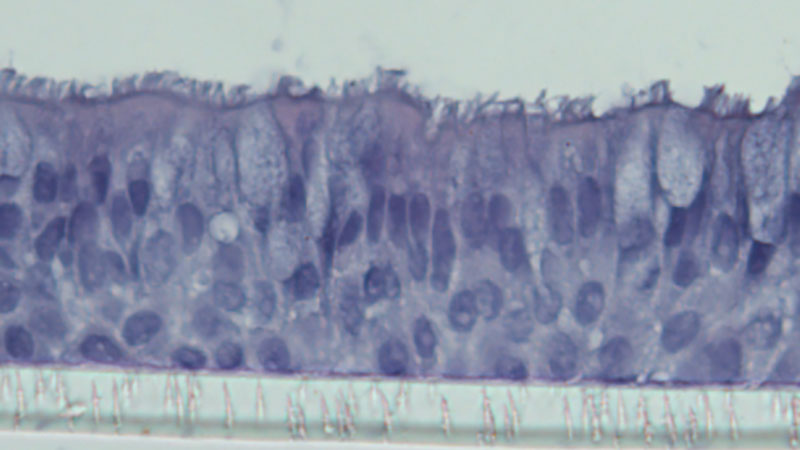
The study used bronchial airway cells from children with and without asthma obtained from the airway epithelial cell (the cellular lining of the airway) biorepository of Dr. Jason Debley, CRBT interim director and principal investigator and professor of pediatrics, University of Washington School of Medicine.
Members of the Debley Lab, including Lucille Rich, Elizabeth Vanderwall and Maria White, conducted SARS-CoV-2 infection experiments with the cells in the research institute’s biosafety level 3 facility using a unique airway model that closely mimics the cell types and function of the human airway, the initial site of SARS-CoV-2 infection. Results demonstrated the virus multiplied less in airway epithelial cells from children with allergic asthma compared to their healthy counterparts, and that increasing the level of type-2 inflammation in the epithelium dramatically weakened viral replication.
“This was a team-science collaborative effort involving investigators from multiple institutions that has identified novel cellular and molecular mechanisms whereby children with allergic asthma are likely protected from SARS-CoV-2 infection,” said Debley, co-senior author of the paper. “Early epidemiologic and clinical studies reported conflicting results about whether asthma was a risk factor for severe COVID-19 disease.
“As the pandemic progressed, clinical data from around the world more consistently, yet counterintuitively, suggested that allergic asthma in children and young adults either conferred no increased risk or even provided modest protection against COVID-19. Our study provides novel mechanistic insights explaining intrinsic protection against SARS-CoV-2 in the airways of patients with allergic type-2 asthma that is consistent with those clinical observations,” he said.
“This is perhaps the most compelling demonstration of a mechanism of intrinsic protection against SARS-CoV-2,” said BRI affiliate investigator and study co-author Dr. Matthew Altman in a BRI news release. “We know antibody responses after vaccine or natural infection are protective, but this mechanism protects in the absence of prior exposure to the virus.”
The study was funded by the National Institute of Allergy and Infectious Diseases, National Institutes of Health.
— Colleen Steelquist
