Eldredge Lab
Modeling Airway Epithelial Cell Differentiation and Injury in BPD
The Eldredge Lab's mission is to study novel mechanisms of bronchopulmonary dysplasia (BPD) pathogenesis.
BPD is a chronic (and likely life-long) lung disease that develops after premature birth. There are neither reliable predictors of individual pulmonary outcomes nor targeted therapeutics to alter BPD progression. BPD affects alveolar, vascular and airway respiratory compartments. Airway disease in BPD is associated with increased mortality, respiratory treatment needs and poor respiratory outcomes such as invasive mechanical ventilation.
There are three areas of research in the Eldredge Lab:
- Development of airway disease in severe BPD (Seattle Children's clinical research, BPD Collaborative)
- Hyperoxia-induced lung injury in vivo (basic mouse model)
- Airway epithelial cell differentiation (mechanistic translational model)
Our longer-term goals are to understand which infants develop BPD-related airway disease, when airway epithelial injury occurs during BPD pathogenesis and what we can do to prevent and/or treat this BPD phenotype.
Airway Epithelial Cell Differentiation and Injury in Bronchopulmonary Dysplasia
 Bronchopulmonary dysplasia (BPD) is a chronic lung disease of extremely premature infants. Airway injury, remodeling and obstruction contribute to BPD pathogenesis. Modeling airway epithelial differentiation is important as samples from critically ill infants are difficult to obtain, and airway disease remains an understudied yet physiologically relevant element therein.
Bronchopulmonary dysplasia (BPD) is a chronic lung disease of extremely premature infants. Airway injury, remodeling and obstruction contribute to BPD pathogenesis. Modeling airway epithelial differentiation is important as samples from critically ill infants are difficult to obtain, and airway disease remains an understudied yet physiologically relevant element therein.
In this project we are using a combination of in vivo and ex vivo approaches:
- Investigating molecular pathways differentially expressed by tracheal epithelial cells from infants with evolving BPD
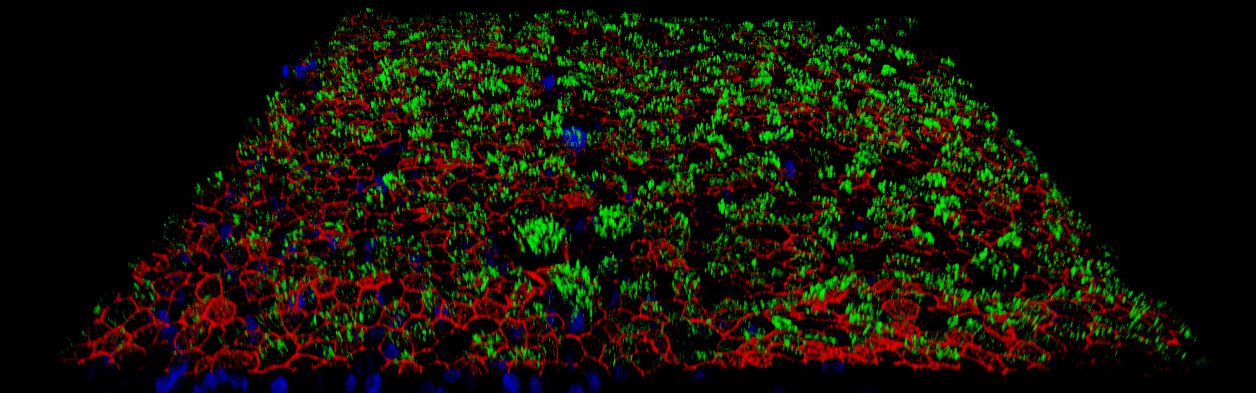
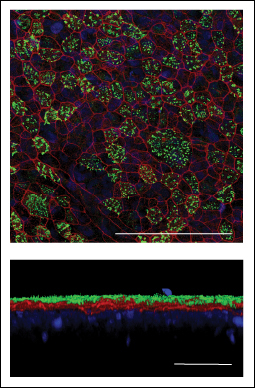
- Characterizing the ex vivo growth and differentiation properties of BPD airway epithelia using an organotypic AEC culture model
- Studying the impact of hyperoxia-induced airway epithelial injury ex vivo
- Describing airway epithelial structure in pathologic specimens from patients who died with evolving severe BPD (collaboration with Deutsch Lab)
The Role of IL-33 Signaling in Airway Epithelial Cell Development and Repair in BPD
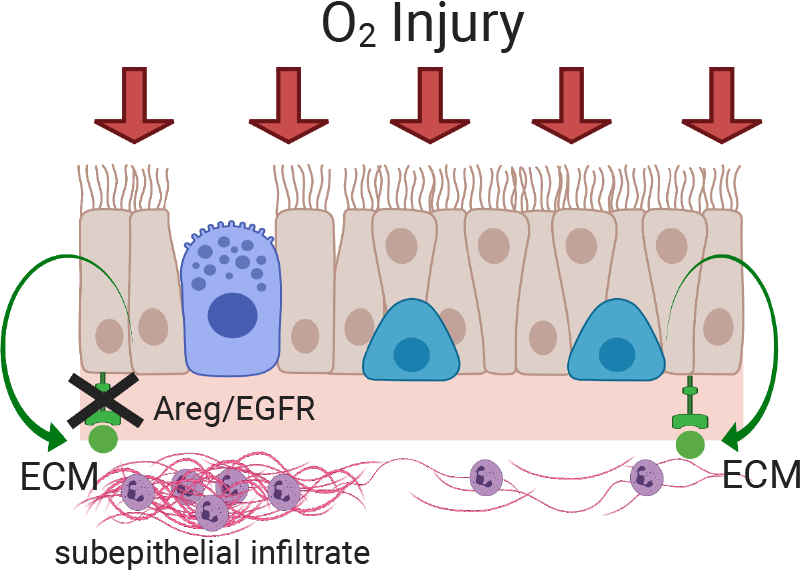
We study type 2 inflammation and the IL-33/amphiregulin (Areg) axis in the developing lung. Areg is an EGF family member that governs epithelial repair through promoting extracellular matrix deposition as well as expression of proteases, but its role in neonatal lung injury is unknown. We hypothesize that Areg is critical for airway epithelial cell differentiation, altering barrier integrity and ECM production during neonatal lung injury. This project uses a comparative medicine approach with neonatal mice and samples from premature infants.

Laurie Christine Eldredge, MD, PhD
Dr. Eldredge is an assistant professor in the Department of Pediatrics at the University of Washington School of Medicine and an attending physician at Seattle Children’s Hospital. She earned her MD and PhD at Northwestern University Feinberg School of Medicine in Chicago. She completed pediatrics residency training and a fellowship in pediatric pulmonology at the University of Washington. Her fellowship and postdoctoral work in neonatal pulmonary immunology was mentored by Dr. Steven Ziegler at Benaroya Research Institute. She joined Seattle Children’s Research Institute and the Center for Respiratory Biology and Therapeutics in 2023 to focus on neonatal airway epithelial cell development and injury.
-
Yan Han, PhD
Research Scientist
Dr. Han brings exceptional experience in tissue engineering, multidimensional confocal microscopy, and developing organotypic cell culture models to the lab.
