Explore Our Research
Oral Airway Plate
 Children with craniofacial abnormalities, such as Robin syndrome, often face severe breathing problems due to small jaws, tongues and cleft palates. While typical treatment emphasizes surgical advancement of the jaw, growing evidence supports the use of an oral airway plate (OAP) to improve breathing, feeding, sleep and growth. As part of a multidisciplinary team at Seattle Children’s spanning critical care, craniofacial surgery, otolaryngology and dental specialties, we have developed novel analytic methods to better analyze airway features and create custom OAP bending devices using 3D printing. We have also developed workflows for generating customized tracheostomy tube shapes, offering enhanced support for patients with complex anatomy and non-standard devices.
Children with craniofacial abnormalities, such as Robin syndrome, often face severe breathing problems due to small jaws, tongues and cleft palates. While typical treatment emphasizes surgical advancement of the jaw, growing evidence supports the use of an oral airway plate (OAP) to improve breathing, feeding, sleep and growth. As part of a multidisciplinary team at Seattle Children’s spanning critical care, craniofacial surgery, otolaryngology and dental specialties, we have developed novel analytic methods to better analyze airway features and create custom OAP bending devices using 3D printing. We have also developed workflows for generating customized tracheostomy tube shapes, offering enhanced support for patients with complex anatomy and non-standard devices.
Papers
Clements AC, Evans SS, Mockler B, Richardson C, Bly RA, Johnson KE, Friedman SD, Dahl JP, et al. Outcomes of Virtually Assisted Personalized Tracheostomy Tubes for Congenital Airway Anomalies. Laryngoscope. 2025. Epub 20250512. doi: 10.1002/lary.32257. PubMed PMID: 40353737.
Evans SS, Richardson C, Friedman SD, Bly RA, Johnson KE, Dahl JP, Parikh SR, Bonilla-Velez J. Virtually Assisted Personalized Tracheostomy Tube Design in Pediatric Complex Airway Anomalies. Otolaryngol Head Neck Surg. 2023;168(4):893-7. doi: 10.1177/01945998221126180. PubMed PMID: 36125892; PMCID: PMC10243722.
3D Printing and Surgical Simulation
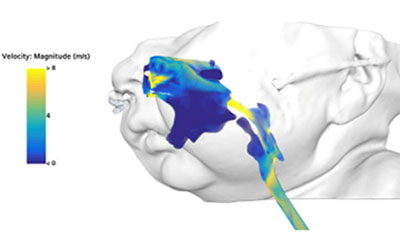
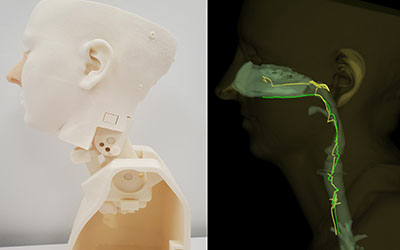 The 3D Lab is advancing surgical simulation in congenital airway diseases by designing and printing multi-material constructs based on biological tissue testing. Computational flow modeling is also used to predict how surgical approaches affect airflow parameters. These innovations are now brought yearly to national and international conferences, training a new generation of surgeons. The lab also develops novel endoscopy trainers that incorporates tool tracking and digital twin counterparts for optimizing skill acquisition in pediatric and adult simulation programs. Current research focuses on understanding the benefits of real-time auditory feedback and gamification (e.g. adding a leaderboard to see who performs best) to improve learner proficiency.
The 3D Lab is advancing surgical simulation in congenital airway diseases by designing and printing multi-material constructs based on biological tissue testing. Computational flow modeling is also used to predict how surgical approaches affect airflow parameters. These innovations are now brought yearly to national and international conferences, training a new generation of surgeons. The lab also develops novel endoscopy trainers that incorporates tool tracking and digital twin counterparts for optimizing skill acquisition in pediatric and adult simulation programs. Current research focuses on understanding the benefits of real-time auditory feedback and gamification (e.g. adding a leaderboard to see who performs best) to improve learner proficiency.
Papers
Richardson CM, Barbour MC, Friedman SD, Parikh SR, Dahl JP, Aliseda A, Johnson KE. Comparison of Postoperative Airflow Changes in Slide Tracheoplasty Across Surgical Techniques Using Computational Fluid Dynamics. Otolaryngol Head Neck Surg. 2025. Epub 20250602. doi: 10.1002/ohn.1330. PubMed PMID: 40454900.
Fernández-Penny FE, Clements AC, Meyer TK, Le H, Bindschadler M, Friedman SD, Sardesai MG. Feedback Enhances Training and Elicits Biometric Responses in Novel Flexible Nasolaryngoscopy Model. Laryngoscope. 2025. Epub 20250508. doi: 10.1002/lary.32231. PubMed PMID: 40342043.
Siu J, Richardson CM, McMullan DM, Files M, Friedman S, Parikh S, Johnson K. Creating Patient-Specific 3D-Printed Airway Models for Slide Tracheoplasty. Laryngoscope. 2024. doi: 10.1002/lary.31435. PubMed PMID: 38771117.
Endoscopy Reconstruction
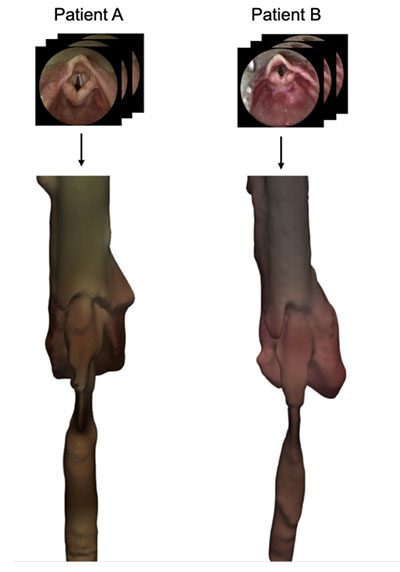 Accurate quantification of airway features is essential for accurate diagnosis and management over time. The main method used for airway visualization is endoscopy, which can provide qualitative data for diagnostic decision-making, but does not allow generation of 3D quantitative surfaces like computed tomography (CT). To overcome the radiation risk of CT and allow a method that would be optimal for serial monitoring, we developed a novel video reconstruction approach using target calibration and Structure from Motion algorithms. By extracting quantitative data from endoscopy videos, this method offers a safer and more effective way to monitor airway changes over time, enhancing diagnostic accuracy and therapeutic monitoring.
Accurate quantification of airway features is essential for accurate diagnosis and management over time. The main method used for airway visualization is endoscopy, which can provide qualitative data for diagnostic decision-making, but does not allow generation of 3D quantitative surfaces like computed tomography (CT). To overcome the radiation risk of CT and allow a method that would be optimal for serial monitoring, we developed a novel video reconstruction approach using target calibration and Structure from Motion algorithms. By extracting quantitative data from endoscopy videos, this method offers a safer and more effective way to monitor airway changes over time, enhancing diagnostic accuracy and therapeutic monitoring.
Papers
Barbour MC, Amin SN, Case HF, Friedman SD, Perez FA, Bly RA, Johnson KE, Parikh SR, Richardson CM, Dahl JP, Aliseda A. Structure From Motion Reconstruction of the Pediatric Larynx: A Clinical Case Series. Otolaryngol Head Neck Surg. 2025. Epub 20250410. doi: 10.1002/ohn.1247. PubMed PMID: 40211657.
Barbour MC, Amin SN, Friedman SD, Perez FA, Bly RA, Johnson KE, Parikh SR, Richardson CM, Dahl JP, Aliseda A. Surface Reconstruction of the Pediatric Larynx via Structure from Motion Photogrammetry: A Pilot Study. Otolaryngol Head Neck Surg. 2024;170(4):1195-9. doi: 10.1002/ohn.635. PubMed PMID: 38168480; PMCID: PMC10960702.
Grant
NIH R21 (2024-2025): 5R21HL172011-03, Computer-Vision and Computational Fluid Dynamics Analysis Pipeline to Improve Diagnosis in Pediatric Subglottic Stenosis (PI Barbour)
Imaging Quantification
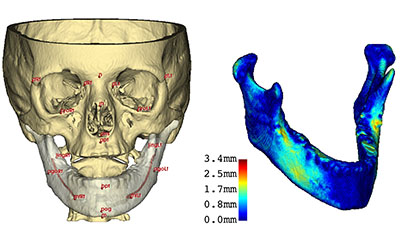 The team leads numerous imaging-based quantification studies focused on diagnostic assessment and therapeutic monitoring. Recent projects include developing image processing methods to quantify tracheomalacia (airway softening) from CT, using atlas-based methods to study how cleft palate affects jaw growth and facial symmetry, microCT of airway tissues, integrating imaging and genetic data to advance epilepsy research, applying artificial intelligence and machine learning to track disease progression in muscular dystrophy, and creating novel tissue-classification approaches to monitor T-cell brain tumor therapy.
The team leads numerous imaging-based quantification studies focused on diagnostic assessment and therapeutic monitoring. Recent projects include developing image processing methods to quantify tracheomalacia (airway softening) from CT, using atlas-based methods to study how cleft palate affects jaw growth and facial symmetry, microCT of airway tissues, integrating imaging and genetic data to advance epilepsy research, applying artificial intelligence and machine learning to track disease progression in muscular dystrophy, and creating novel tissue-classification approaches to monitor T-cell brain tumor therapy.
Papers
Case HF, Bindschdler M, Barbour M, Meyer T, Dahl JP, Friedman SD, Aliseda A, Bly RA. Dynamic Airway CT for Morphometric Analysis of Pediatric Tracheomalacia Throughout Respiration. Otolaryngol Head Neck Surg. 2025. Epub 20250521. doi: 10.1002/ohn.1313. PubMed PMID: 40396449.
Blemker SS, Riem L, DuCharme O, Pinette M, Costanzo KE, Weatherley E, Statland J, Tapscott SJ, Wang LH, Shaw DWW, Song X, Leung D, Friedman SD. Multi-scale machine learning model predicts muscle and functional disease progression. Sci Rep. 2025;15(1):25339. Epub 20250716. doi: 10.1038/s41598-025-09516-8. PubMed PMID: 40670422; PMCID: PMC12267502.
Tse RW, Sitzman TJ, Allori AC, Ettinger RE, Fisher DM, Bezuhly M, Samson TD, Beals SP, Matic DB, Mercan E. Measuring the Unilateral Cleft Lip Nasal Deformity: Lateral Deviation of Subnasale Is a Clinical and Morphologic Index of Unrepaired Severity. Cleft Palate Craniofac J. 2025;62(1):69-78. Epub 20231003. doi: 10.1177/10556656231202173. PubMed PMID: 37787163.
Straccia A, Barbour MC, Chassagne F, Bass D, Barros G, Leotta D, Sheehan F, Sharma D, Levitt MR, Aliseda A. Numerical Modeling of Flow in the Cerebral Vasculature: Understanding Changes in Collateral Flow Directions in the Circle of Willis for a Cohort of Vasospasm Patients Through Image-Based Computational Fluid Dynamics. Ann Biomed Eng. 2024;52(9):2417-39. doi: 10.1007/s10439-024-03533-w. PubMed PMID: 38758460; PMCID: PMC11329356.
Pirozzi F, Berkseth M, Shear R, Gonzalez L, Timms AE, Sulc J, Pao E, Oyama N, Forzano F, Conti V, Guerrini R, Doherty ES, Saitta SC, Lockwood CM, Pritchard CC, Dobyns WB, Novotny E, Wright JNN, Saneto RP, Friedman S, Hauptman J, Ojemann J, Kapur RP, Mirzaa GM. Profiling PI3K-AKT-MTOR variants in focal brain malformations reveals new insights for diagnostic care. Brain. 2022;145(3):925-38. doi: 10.1093/brain/awab376. PubMed PMID: 35355055; PMCID: PMC9630661.
Grants
NINDS U01 (2024-2029): U01NS137702. Title: Motor Outcomes to Validate Evaluations in Pediatric FSHD (MOVE Peds) (PI STATLAND J, EICHINGER K, FRIEDMAN SD, WOODCOCK I)
NIH U54 (2023-2028): U54AR065139; Title: Paul D. Wellstone Muscular Dystrophy Cooperative Research Center (PI: CHAMBERLAIN J, TAPSCOTT S (Friedman SD - co-investigator))
NIH 1R01CA289981-01 (2024-2029): Title: Clinical translation of B7H3-PD1:MyD88 CART cells for children and young adults with diffuse midline glioma. PI: VITANZA N (Friedman SD, Bindschadler M, Mercan E - co-investigators)
