Explore Our Research
Solid Tumors
The self-protective features presented by solid tumors are more difficult to overcome than the roadblocks presented by blood tumors. It’s a major reason why adoptive cell therapy is further along for blood cancers than for many solid tumors.
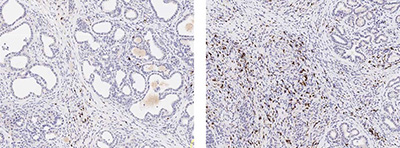
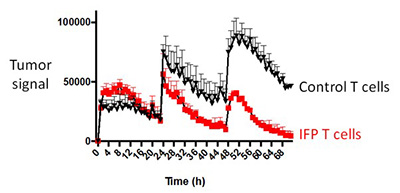
One of the barriers presented by solid tumors is T cell exhaustion. Normal T cells, as well as T cells that are modified with adoptive cell therapies such as CAR T, become exhausted before they are able to mount a sustained attack on tumor cells. Using IncuCyte technology, we are able to observe how the T cells modified with FPs behave over time in a setting that mirrors a human environment. This allows us to measure the durability of a T cell’s killing response to wave after wave of tumor cells. Animal models with our FP-enhanced cell therapy were able to destroy repeated additions of tumor cells, whereas control T cells became dysfunctional and ineffective.
The “shut off” message that solid tumor cells send tells the T cells to self-destruct. The cancer cells even scatter the deadly messages at the edge of blood vessels, so some of the T cells die before they can reach the tumor. The FP we’ve crafted for our solid tumor studies rewires the T cells to interpret the negative message as one that stimulates their cancer-killing abilities.
We have engineered a FP that combines a death receptor ectodomain, Fas, with the pro-survival costimulatory 4-1BB signaling domain, converting a death signal to an activation boost for T cells. We showed that the Fas-41BB FP supported improved survival in several models of solid tumors. We are excited to determine the tumor microenvironment obstacles that FPs can overcome and extend these findings to create effective tumor immunotherapies.
Catalyzing Endogenous Antitumor Immunity with Dual Costimulatory Receptors (DCR)
 (Image created with biorender.com)
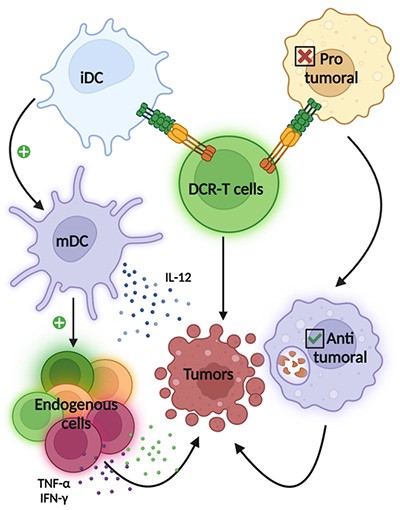
(Image created with biorender.com)Adoptive cell therapy (ACT) is an exciting therapeutic strategy that uses genetically-engineered immune cells to target and destroy tumors. However, engineering strategies to enhance ACT typically focus only on improving the cell “product” and do not provide support for immune cells that are already in the patient.
We innovate fusion proteins that combine a membrane-bound protein ectodomain with a costimulatory signaling endodomain. These novel proteins are expressed in genetically engineered T cells, for use in cell therapy.
We are developing a new class of fusion proteins, called Dual Costimulatory Receptors (DCR), that combine a costimulatory ligand ectodomain with a different costimulatory signaling endodomain. The DCR ectodomain has the potential to stimulate costimulatory receptors on the T cell and endogenous immune cells, and the intracellular domain can be used to provide costimulatory signals only to the T cell (signals that are not safe to deliver systemically). As tumor-targeted T cells actively migrate to the tumor site, DCRs will provide safer, localized delivery of positive signals to endogenous immune cells and a more powerful engineered T cell response.
We are developing DCRs to catalyze a diverse antitumor response against a broad range of cancers.
