Oda Lab
Replacing Cancer’s Brake With a T-cell Accelerator
The Oda Lab develops engineering strategies that enable T cells to overcome obstacles in the tumor microenvironment and mount a more powerful, durable and sustained attack on cancer cells.
Cancer cells and the microenvironment they create can set up barriers that block effective immunotherapy treatment. They send out signals that interfere with the activation of T cells specifically recognizing cancer, as well as cause T cells to self-destruct before they can do their job.
Our research augments the efficacy of adoptive cell therapy (ACT), a promising immunotherapy treatment option that uses genetically modified immune cells (T cells) to eliminate tumors. To create cell therapies, a small number of T cells are removed from the patient’s blood, their genetic instructions are changed to more effectively fight cancer, and then the T cells are infused back into the patient to seek out and destroy tumor cells.
While encouraging results have been obtained by adoptive cell therapies, their efficacy is dampened by the protective behaviors of cancer tumors. Tumor cells send signals in the form of inhibitory proteins to T cells, which prevent them from becoming fully activated and, in many cases shut them down altogether.
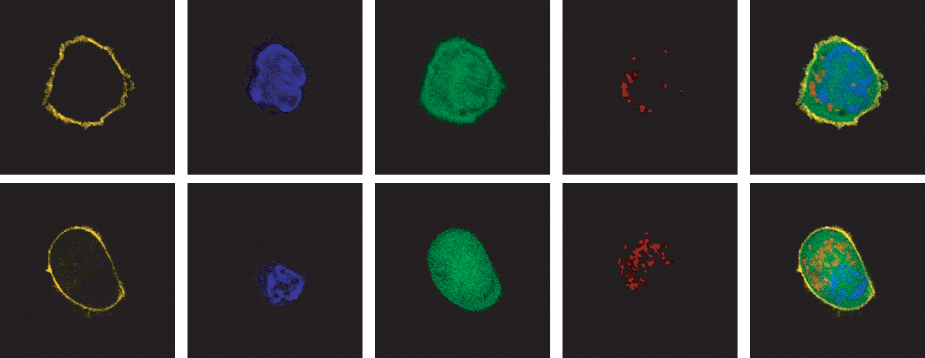
Our laboratory focuses on making the next generation of immunotherapies more effective and applicable to patients. We have engineered new types of hybrid proteins called fusion proteins (FPs). When FPs are added to adoptive cell therapy, they boost T cells’ ability to respond aggressively to tumors and completely bypass what is normally an inhibitory or death signal from cancer cells.
Our research applies to tumor microenvironments that are present in many different kinds of cancers. We are developing our technology for blood tumors, including acute myeloid leukemia (AML), as well as solid tumors, including pancreatic, ovarian, brain, and lung cancers.
We are excited to discover that FPs give T cells a boost that impacts many different functions, such as enhanced metabolism, lowered threshold of activation, reduced exhaustion, and increased intratumoral concentration. This single addition may help immunotherapy treatments bypass multiple tumor barriers. Our research aims to dramatically improve cell therapies for multiple cancer types with intentionally engineered proteins.
Explore Our Research
Partnership Opportunities

Shannon Oda, PhD
Dr. Shannon Oda earned a PhD in immunology from the University of Colorado Anschutz Medical Campus and National Jewish Health and completed her postdoctoral training with Dr. Philip Greenberg at the Fred Hutch Cancer Center. She has received several awards, including the Future of Science Award and the LLS Career Development Program Special Fellow Award, and has been invited to give talks internationally.
Oda joined Seattle Children's Research Institute in 2020, where she is an assistant professor at the Ben Towne Center for Childhood Cancer and Blood Disorders Research and the University of Washington School of Medicine. Her research focuses on improving T-cell immunotherapy, which uses immune cells to target and destroy cancer cells. She has identified several obstacles that inhibit immune cells from effectively eradicating tumor and she is inventing new ways to engineer T cells to overcome these obstacles and improve immunotherapy of hematological and solid tumors.
@ShannonKOda (X)
-

Simonne Guenette
Graduate Student
-

Vijini Liyanage
Student
-

Aidan Schutte
Student
-

Ryma Toumi, PhD
Research Scientist II
