Research Provides Immediate Improvements to Administration of Delirium Assessment Tool at Seattle Children’s
Pediatric delirium is not something widely discussed outside the walls of a pediatric intensive care unit (PICU), but for pediatric critical care providers, it’s a very real risk they confront every day. Delirium is a serious complication of hospitalization and in children can present itself through behavior such as restlessness and agitation, visual or auditory hallucinations, lethargy or generally children “not being themselves.” Critical illness is the most common cause of delirium in children, and a delirium diagnosis in children has been associated with an increase in length of stay and number of days of mechanical ventilation, as well as increased mortality.

Hector Valdivia, Clinical Nurse Specialist in Seattle Children’s Pediatric Intensive Care Unit
Pediatric delirium is a relatively new field within pediatrics, and the prevalence is still being explored. Two tools are available to care providers to screen for delirium – the Cornell Assessment of Pediatric Delirium (CAPD) and the Pediatric Confusion Assessment Method ICU (pCAM-ICU). Seattle Children’s utilizes the CAPD tool to assess delirium in patients in our PICU. For PICU Clinical Nurse Specialist Hector Valdivia, recognizing that we have patients in our ICU and PICU experiencing some form of delirium is the first step. “While it’s important to have a tool available to help us assess delirium in our patients,” says Hector, “the consistency of administration of the tool is equally important – will we get the same results when the tool is administered by different people?”
This line of thinking prompted Hector to design a research study assessing the interrater reliability – the frequency the same result would occur – of the CAPD tool among PICU nurses.
Patients from Seattle Children’s PICU and Cardiac Intensive Care Unit (CICU) were eligible to participate and a total of 108 patients were included in the study. To gather results, a nurse researcher observed a clinical nurse administer the CAPD tool, which is a standard screening procedure administered at noon and midnight in the PICU and CICU. Within an hour of the initial observation, the nurse researcher would also complete the CAPD screening procedure with the same patient. Data from the observations and tool results were analyzed by biostatistician Kristen Carlin.
The results of the study, published in the Pediatric Critical Care Medicine journal, indicated there was strong agreement in CAPD results between research and clinical nurses in patients over 2 years of age, while there was not agreement between nurses for patients less than 2 years old.
According to Hector, these results are not too surprising. “We found that there could be differences in how the questions were interpreted,” says Hector. “One of the anchor questions is ‘was the patient’s movement purposeful’ – if you apply that to a 10 year old you have a better idea of what a typical 10 year old’s movements should be. In a 2 month old, it’s much harder to answer and leaves more to interpretation.”
The CAPD provides reference points or general guidelines for what to look for when administering the tool for children under 2 to help address the issue of interpretation. However, the reference points are not easily accessible to the nurse administering the tool, requiring several clicks within the tool to find them.
Based on the study finding, changes were implemented at Children’s in how nursing staff view the CAPD tool, specifically for children younger than 2.
“We placed the reference points directly in the tool for each question so nurses don’t have to click anywhere to receive the guidance,” says Hector. “We also created individual CAPD tools for each age group under 2 so nurses only see the guidance for the specific age group they are administering the tool to.” The system assigns the age appropriate tool based on the chronologic age in the patient’s electronic health record.
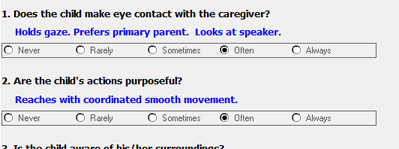
Reference points for a 28-week old, shown in blue in the screenshot above, help nursing staff administer the tool in a more consistent manner, resulting in more consistency in diagnoses of delirium.
In reviewing informatics literature derived from other studies about delirium assessment tools, Hector found there was higher performance of the tools when clinical staff had the necessary information at the point of care and that questions are answered in a more consistent manner, which should result in more consistent diagnoses of delirium in pediatric patients.
The fact that there is still much to be learned about delirium in pediatric patients is energizing to Hector. “We still have a lot to learn about how we assess delirium and how we, as a team, interpret results to then make interventions to reduce the risk of delirium or manage delirium in pediatric ICUs,” says Hector.
“I appreciate the direction we are going at Children’s,” says Hector. “There is a recognition of the importance of research and resources to help facilitate it. As a CNS, an equally important part of being a nurse is research and asking questions and exploring ways we can generate new ideas and improve care for our patients.”
Hector recently contributed as an author to the Society of Critical Care Medicine ICU Liberation, second edition book. The second edition highlights the latest guidelines on the ICU Liberation campaign to reduce complications of ICU admissions.
