Surgery for Hypertonia: A Q&A With Dr. Samuel Browd
July 5, 2023
Samuel Browd, MD, PhD, is a neurosurgeon and surgical director of the Tone Management Program at Seattle Children’s. He is a world leader in training surgeons in selective dorsal rhizotomy (SDR) procedures. Roughly 1 in 4 surgeons in the United States who offer SDR trained under Dr. Browd, in addition to many doctors from around the world.
Q: Who is SDR for?
 Dr. Browd: Any child with high tone (spasticity) in their lower extremities is a possible candidate for SDR [selective dorsal rhizotomy] surgery. This includes many children with cerebral palsy. Providers and parents often think of surgery as a last resort, but in the case of kids with high tone, we encourage them to think of it as an early option instead. Even if their spasticity is being reasonably well-managed by medication and/or therapies, SDR can help them reduce or even get off their medication. With better physical functioning and mobility, we see kids do better with their social, family and school life too — because they’re putting less physical and mental energy into controlling their body and more time into doing things that are fun for them. Longer-term, kids are less likely to require more surgeries or experience some of the serious health consequences of having high tone.
Dr. Browd: Any child with high tone (spasticity) in their lower extremities is a possible candidate for SDR [selective dorsal rhizotomy] surgery. This includes many children with cerebral palsy. Providers and parents often think of surgery as a last resort, but in the case of kids with high tone, we encourage them to think of it as an early option instead. Even if their spasticity is being reasonably well-managed by medication and/or therapies, SDR can help them reduce or even get off their medication. With better physical functioning and mobility, we see kids do better with their social, family and school life too — because they’re putting less physical and mental energy into controlling their body and more time into doing things that are fun for them. Longer-term, kids are less likely to require more surgeries or experience some of the serious health consequences of having high tone.
Ages 3 to 5 is when we like to see kids get evaluated for SDR because their neuroplasticity is so high at that age, but we also consider the surgery for older children.
Q: What happens during surgery?
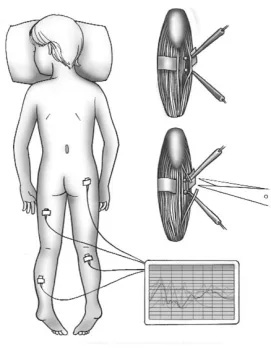 We make a small incision in the child’s back and perform a laminectomy (small window in the spine) to access nerves at the bottom of the spinal cord. We use neuromonitoring to test each nerve and cut those abnormal sensory nerve fibers that are contributing to spasticity. Which nerves and how many are cut vary depending on the patient’s preoperative assessment and the nerve-by-nerve neuromonitoring we’re doing during the surgery. There’s a detailed video presentation of the procedure in a Grand Rounds video I presented recently here: https://care.sc/sdr-gr.
We make a small incision in the child’s back and perform a laminectomy (small window in the spine) to access nerves at the bottom of the spinal cord. We use neuromonitoring to test each nerve and cut those abnormal sensory nerve fibers that are contributing to spasticity. Which nerves and how many are cut vary depending on the patient’s preoperative assessment and the nerve-by-nerve neuromonitoring we’re doing during the surgery. There’s a detailed video presentation of the procedure in a Grand Rounds video I presented recently here: https://care.sc/sdr-gr.
I actually consider the surgery to be the easy part. The harder work lies in the follow-up physical therapy (PT). PT begins in the hospital and continues back in the child’s home community with their local therapist.
Q: You like to say this is your favorite surgery. Why is that?
It’s because the kids do so well afterward, making strides and hitting new milestones that are exciting for them and their family. There’s a lot in the medical literature about the positive outcomes of SDR, but what’s not in the literature is the quality-of-life improvements we hear about that make this surgery life-changing for the patients and families.
Q: What makes a child a good candidate for SDR?
A child with high tone in the lower extremities (with Gross Motor Function Classification System I-III) who has mobility goals and is able to participate in physical therapy is a good candidate for evaluation for surgery.
To determine if SDR surgery is a good option, evaluation is the first step. Our team conducts a comprehensive, two-day assessment of the child that brings together members of our Tone Management Program including myself, a Rehab Medicine provider and our physical and occupational therapists who follow patients postoperatively, who will measure the child’s muscle tone, range of motion and strength to ensure we’re looking at all aspects of the child’s function and participation.
Q: How are you measuring outcomes?
There is so much we want to measure with this population including participation outcomes and subjective satisfaction outcomes. For that reason, we’ve chosen to use a number of objective measurement tools to assess outcomes and compare preoperative to postoperative scores. Two of our favorites are the Gross Motor Functional Measure (measures mobility) and the Cerebral Palsy Gait Outcomes Assessment List (CP GOAL; measures quality of life).
The medical literature shows that SDR offers sustained, durable outcomes between 17 and 26 years [of age] with benefits that include reduced spasticity, improved function and range of motion, improved social functioning and high patient/family satisfaction. On that latter point, parents we have surveyed consistently say they are glad they chose surgery and would do it again.
Q: What do you want other providers to know?
We know there are many kids out in the community with high tone who we’re not seeing. Our request is that you send them to us. If you’re managing a kid with CP [cerebral palsy] in primary care or you’re their PT or OT, please send them to be evaluated. SDR is an important option for them, and they need to know it’s out there.
Resources
- Erin Hooper, RN, BSN, Tone Management Program Manager
- Phone: 206-987-5917
- Email: [email protected]
- Algorithm: Hypertonia
- SDR at Seattle Children’s
- Seattle Children’s Tone Management Program (TMP)
- SDR: Grand Rounds video featuring Dr. Browd, Nov. 2022