Case Study: Chronic Recurrent Multifocal Osteomyelitis (CRMO) Presenting as Bony Pain in a Young Soccer Player
January 5, 2022
Authors: Natalie Rosenwasser and Dan (Yongdong) Zhao
Related Reading: When Bone Pain Isn’t What You Think: Recognizing CRMO in Primary Care, Provider News, December 2021.
Summary
A 12-year-old male presented with chronic bony pain in his left hip and back, for which multiple X-rays were read as normal. An MRI of the pelvis showed concern for CRMO. He was referred to the Rheumatology Clinic and has been doing well on immunosuppressive medications for his CRMO.
Patient History
The patient presented at age 12 to the Orthopedic Clinic at Seattle Children’s for year-long bone pain in his left hip and groin, back, ankle, and knee. The pain started about one year ago and was initially considered mild by him. He was very active in year-round soccer prior to his presentation. At presentation he had pain in the left hip region for the last three weeks. His pain increased after a respiratory illness to the point where he could not participate in sports. He also was noted to be limping. He had no notable trauma.
The pain was worse in the morning and right before bedtime. Activity would worsen his pain, which could recur thereafter. He described 5 to 10 minutes of morning stiffness in his groin. He denied any joint swelling or warmth. Stretching helped to some degree but has not offered dramatic relief of his pain. He had tried anti-inflammatories and rest with little relief. His family noted that he had been less active, less motivated, more tired and more sedentary one month prior to presentation. He denies any rashes, weight loss or fevers.
On exam, he had significant pain in the lateral decubitus position with abduction and external rotation. Trendelenburg was positive. FABER was positive for pain in the anterior groin. He has a positive Thomas test, negative snapping hip, positive Ober, negative FADDIR and negative posterior impingement. He had pain along the iliopsoas and the piriformis. He had a positive piriformis test and no tenderness on SI joints.
He had labs completed by Orthopedics revealing a normal CBC, ESR, CRP, BUN, creatinine, AST and ALT. His ANA screen was negative and his HLA-B27 was positive. Four plain films of his pelvis were completed, which were unrevealing over the course of the year. An MRI of the pelvis without contrast was finally performed but read as “Abnormal marrow edema at the greater trochanters and proximal femoral necks centered around the apophysis. There is a linear high signal along the apophysis. There is suspected periosteal reaction along the femoral shaft; this pattern was highly suggestive of a stress-type response and thought to represent apophysitis.” Given the persistence in symptoms, he was seen by an orthopedist who prescribed physical therapy (PT), which helped him to some degree.
He was referred to Rheumatology due to persistent symptoms despite PT, and the MRI was reviewed with our musculoskeletal radiologists and found to be more consistent with CRMO that typically affects the metaphyses of long bones in a symmetrical pattern.
Patient Diagnosis: Chronic Recurrent Multifocal Osteomyelitis (CRMO)
The patient was initially started on prednisone and meloxicam for pain relief and initial treatment with an H2 blocker and PPI. He eventually required additional immunosuppression with methotrexate, which he, unfortunately, did not tolerate. Adalimumab was prescribed, and leflunomide was added for anti-adalimumab antibody prevention that led to disease remission.
Outcome
The patient had an excellent response to his current medication regimen with dramatic improvement in pain and physical function. He returned to his soccer team and has not had any pain for the last four years while he was on medications.
Imaging
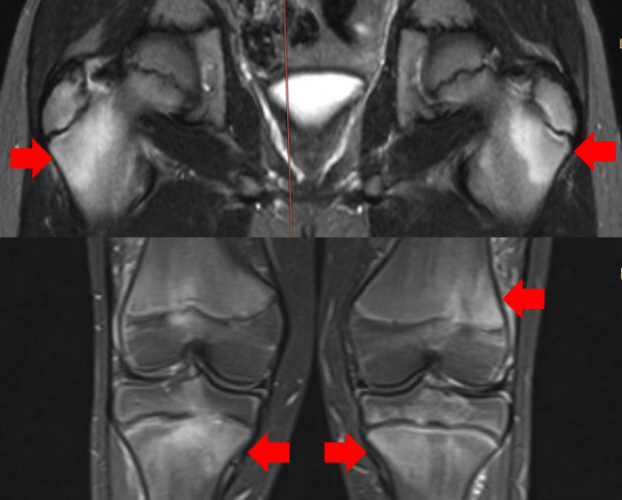 Figure 1: MRI images of Coronal view of pelvis and knees from STIR sequence at initial diagnosis. The top panel shows abnormal marrow signals within both proximal femurs (arrows). The bottom panel shows abnormal marrow signals within both proximal tibias and left distal femur (arrows).
Figure 1: MRI images of Coronal view of pelvis and knees from STIR sequence at initial diagnosis. The top panel shows abnormal marrow signals within both proximal femurs (arrows). The bottom panel shows abnormal marrow signals within both proximal tibias and left distal femur (arrows).
Discussion
CRMO is an autoinflammatory bone disease that affects one or more bones in children. It is occult and difficult to diagnose. Often it is misdiagnosed as growing pain (school-aged children), infectious osteomyelitis (accompanied with fever, elevated inflammation markers), malignancy (abnormal signal on imaging) or overlooked. The majority of patients have a normal joint exam, and X-rays and labs are not sensitive. An MRI is a gold standard for initial diagnostic imaging prior to a whole-body MRI that delineates all affected sites. Prognosis can be significantly improved when a diagnosis is made early and aggressive treatment is initiated accordingly. Our pediatric rheumatology team has a dedicated CRMO clinical program that partners with community physicians to identify these children and provide state-of-the-art treatment plans for them. Please follow this link for details about the program and referral: Chronic Recurrent Multifocal Osteomyelitis Program Seattle Children’s (seattlechildrens.org).
References
- Zhao Y, Dedeoglu F. Chronic nonbacterial osteomyelitis (CNO)/chronic recurrent multifocal osteomyelitis (CRMO). UpToDate 2019.
- Zhao Y, Ferguson PJ. Chronic Non-bacterial Osteomyelitis and Autoinflammatory Bone Diseases. Review. Clinical Immunology. 2020.