Myelomeningocele
-
Schedule an appointment with the Neurosciences Center
If this is a medical emergency, call 911.
- If you would like an appointment, ask your child’s primary care provider for a referral.
- If you have a referral, call 206-987-2016 or 844-935-3467 (toll-free).
- How to schedule.
If you have any questions, please contact us at 206-987-2016 or 844-935-3467 (toll-free).
-
Find a doctor
- Meet the Neurosciences team.
-
Locations
- Seattle Children’s hospital campus: 206-987-2016 or 844-935-3467 (toll-free)
- Bellevue Clinic and Surgery Center: 206-987-2016 or 844-935-3467 (toll-free)
- Everett: 425-783-6200
- Federal Way: 206-987-2016 or 844-935-3467 (toll-free)
- Olympia: 206-987-2016 or 844-935-3467 (toll-free)
- Tri-Cities: 206-987-2016 or 844-935-3467 (toll-free)
- Wenatchee: 206-987-2016 or 844-935-3467 (toll-free)
-
Refer a patient
- Urgent consultations (providers only): call 206-987-7777 or 877-985-4637 (toll free).
- If you are a provider, fax a New Appointment Request Form (NARF) (PDF) (DOC) to 206-985-3121 or 866-985-3121 (toll-free).
- Send the NARF, chart notes and any relevant documentation to 206-985-3121 or 866-985-3121 (toll-free).
- View our complete Neurosciences Center referral guidelines.
What is a myelomeningocele?
A myelomeningocele (my-elo-men-IN-go-seal) is a defect of the backbone (spine), spinal cord and spinal canal. A myelomeningocele (also called MMC) is the most serious form of spina bifida.
This is how myelomeningoceles form in a developing baby before birth. As the fetus grows during pregnancy:
- The bones of the spine (vertebrae) do not form the normal way.
- A small sac containing parts of the spinal cord and nerves pushes through the open bones and sticks out the fetus’s back.
- A myelomeningocele can happen anywhere along the spinal cord. It is most common in the lower back.
- Nerves below the level of the myelomeningocele are damaged. This can affect your baby’s feeling, movement and bladder and bowel control.
- A myelomeningocele higher in the spine results in more severe symptoms.
Doctors do not know the exact cause of myelomeningoceles. Research suggests that genes and nutrients during pregnancy play a role. Getting enough folic acid early in pregnancy can help prevent spina bifida. This B vitamin helps the baby’s neural tube grow properly into the brain and spinal cord.
Why choose Seattle Children's for myelomeningocele care?
 Seattle Children’s has been a leader for 50 years in providing complete, coordinated care for children with myelomeningoceles.
Seattle Children’s has been a leader for 50 years in providing complete, coordinated care for children with myelomeningoceles.
- If a myelomeningocele is detected during pregnancy, specialists at our Fetal Care and Treatment Center will assess your baby’s health to prepare for their birth and care.
- We work closely with your birth hospital and are national leaders in safely moving fragile newborns. Within 1 to 2 days after birth, our skilled neurosurgeons will repair your baby’s spinal defect.
- Our Level 4 (IV) Neonatal Intensive Care Unit (NICU) team is skilled and equipped to care for the sickest newborns. We provide specialized care in our Neuro NICU — the only neonatal neurocritical care program in Washington, Wyoming, Alaska, Montana and Idaho.
- Children with this form of spina bifida often need care for other complex problems. We have a great deal of experience caring for these conditions, such as spinal deformities, hydrocephalus, tethered spinal cord, Chiari malformation and syringomyelia.
- Nerve damage from the myelomeningocele can affect your child their entire life. Our Spina Bifida clinic provides ongoing medical and developmental care to children from birth through 21 years of age. Our team includes experts in Neurodevelopment, Neurosurgery, Nutrition, Orthopedics, Rehabilitation Medicine, Urology and Social Work.
- Our Fetal Care and Treatment Center coordinates with other hospitals if you choose surgery to fix the defect during pregnancy.
"Out of all the priceless gifts our care teams have given us, there’s one that sustains us: the simple belief that our son has boundless potential.” - Whitney Stohr, mom of Malachi, who was diagnosed with myelomeningocele during pregnancy. Today, he’s thriving. Read Malachi's story.
What are the symptoms of myelomeningocele?
In a baby with a myelomeningocele, a sac holding parts of the spinal cord pushes out through their back. A myelomeningocele is most common in the lower back. The higher the myelomeningocele is on your baby’s spinal cord, the more nerve damage it causes.
Your child may have:
- Problems moving parts of the body below the opening in the back
- Lack of sensation in their legs and feet
- Poor or no bowel and bladder control
- Twisted or abnormal legs and feet, such as, clubfoot
- A buildup of cerebrospinal fluid (CSF) in the head (hydrocephalus)
- Problems with how the back of the brain formed (Chiari 2 malformation)
- Learning differences or delayed developmental milestones
How is myelomeningocele diagnosed?
Often, a doctor detects the condition during regular pregnancy screenings such as blood tests and ultrasound scans. You may have other tests to confirm the diagnosis.
If a doctor confirms your fetus has a myelomeningocele, they may refer you to our Fetal Care and Treatment Clinic. Our team will check your baby’s health and do imaging studies such as MRI (magnetic resonance imaging) and ultrasound. After a full assessment, we will advise you on what to expect. We’ll work with your birth hospital to plan for your baby’s delivery and the treatment they will need.
Sometimes a myelomeningocele is not diagnosed until after a baby is born, when the sac holding the spinal cord is seen pushing through the baby’s back. We may order imaging tests to assess their spine and plan treatment.
How is myelomeningocele treated?
Surgery to repair the defect in your baby’s spinal column is just the first step in their treatment. Your child’s neurosurgeon will work closely with other experts at Seattle Children’s to assess all your child’s needs. Our Spina Bifida clinic provides coordinated care from birth through 21 years. Each child is different, and we will tailor treatment for your child and family.
Surgery to Repair Myelomeningocele
Fetal surgery
In some cases, neurosurgeons can close the spinal defect during pregnancy. The procedure options are called fetoscopic myelomeningocele repair or in utero open MMC repair. The surgery is done around the 24th week of pregnancy. Seattle Children’s does not offer fetal closure at this time, but plans to provide this surgery in the future. If you choose to have your baby’s MMC repaired during pregnancy, we will work with the center of your choice to coordinate your baby’s care. Some women deliver their baby at the center that performed fetal surgery. Others return to Seattle for delivery. Regardless of delivery location, Seattle Children’s can provide your baby’s ongoing healthcare related to spina bifida.
Surgery after birth
We work closely with your birth hospital to safely transfer your baby to Seattle Children’s soon after they are born. Within your baby’s first 48 hours of life, our experts do surgery to cover and protect your baby’s spinal cord. This:
- Limits the risk of infection
- Prevents more damage to the spinal cord but does not restore damaged nerves

The child is in position for the repair of his spina bifida.
During surgery:
- First, the neurosurgeon closes the covering around the spinal cord.
- Next, the neurosurgeon and plastic surgeon close the muscles and fascia over the spinal cord.
- Finally, they close the skin over the open area.
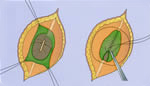
Closing the spinal cord defect in spina bifida.
Treating Related Conditions
Some children with myelomeningoceles have other conditions that need treatment, such as:
- Hydrocephalus, where too much CSF collects in their head and puts pressure on their brain. Most often, neurosurgeons place a tube (called a shunt) in the skull to drain CSF to another part of the body, where it is absorbed.
- Tethered spinal cord, where the spinal cord is pulled down and stuck to the spinal canal instead of floating freely inside it.
- Chiari malformation, a problem with the way parts of the brain are shaped and how they sit in the skull. Parts of the brain hang down through the opening in the base of the skull into the upper neck.
- Syringomyelia, a cyst in the center of the spinal cord that is filled with fluid. This can put pressure on the spinal cord and cause nerve damage.
Ongoing Care
Often, children with myelomeningoceles have complex problems such as limited movement, sensation, or bowel and bladder control. Our Spina Bifida clinic cares for children born with spina bifida from birth through 21 years of age. We design a treatment plan just for your child to meet their needs over the long term.
- Nerve damage often limits movement. If your child has mobility problems, our Orthopedics, Orthotics and Rehabilitation Medicine specialists will work with your child to meet their needs. Treatment options include orthopedic surgery, physical therapy, occupational therapy and aids like braces, crutches or wheelchairs.
- Some children born with a myelomeningocele have differences in their legs, feet, hips or spine. Your child may have orthopedic surgery for problems like clubfoot, curved spine (scoliosis), contracted muscles or dislocated hips.
- In many kids with spina bifida, their bladder does not work normally, because their spinal cord and the nerves that control the bladder did not form correctly before birth. This can affect how their kidneys work, their ability to pee and their quality of life. Seattle Children’s takes part in a nationwide study (UMPIRE) to evaluate the best ways to manage bladder and kidney issues for newborns and young children with spina bifida.
- To address bowel and bladder issues, your child may see specialists in Neurodevelopment, Rehabilitation Medicine, Urology or Gastroenterology.
As they reach adulthood, we help your child transition to a provider who cares for adult patients.
Contact Us
If you would like an appointment, ask your child’s primary care provider for a referral. If you have a referral, call 206-987-2016 to make an appointment.
Providers, see how to refer a patient.
If you have questions, contact us at 206-987-2016 or 844-935-3467 (toll free).
Paying for Care
Learn about paying for care at Seattle Children’s, including insurance coverage, billing and financial assistance.
For Healthcare Professionals
-
Schedule an appointment with the Neurosciences Center
If this is a medical emergency, call 911.
- If you would like an appointment, ask your child’s primary care provider for a referral.
- If you have a referral, call 206-987-2016 or 844-935-3467 (toll-free).
- How to schedule.
If you have any questions, please contact us at 206-987-2016 or 844-935-3467 (toll-free).
-
Find a doctor
- Meet the Neurosciences team.
-
Locations
- Seattle Children’s hospital campus: 206-987-2016 or 844-935-3467 (toll-free)
- Bellevue Clinic and Surgery Center: 206-987-2016 or 844-935-3467 (toll-free)
- Everett: 425-783-6200
- Federal Way: 206-987-2016 or 844-935-3467 (toll-free)
- Olympia: 206-987-2016 or 844-935-3467 (toll-free)
- Tri-Cities: 206-987-2016 or 844-935-3467 (toll-free)
- Wenatchee: 206-987-2016 or 844-935-3467 (toll-free)
-
Refer a patient
- Urgent consultations (providers only): call 206-987-7777 or 877-985-4637 (toll free).
- If you are a provider, fax a New Appointment Request Form (NARF) (PDF) (DOC) to 206-985-3121 or 866-985-3121 (toll-free).
- Send the NARF, chart notes and any relevant documentation to 206-985-3121 or 866-985-3121 (toll-free).
- View our complete Neurosciences Center referral guidelines.