Chiari Malformation
-
Schedule an appointment with the Neurosciences Center
If this is a medical emergency, call 911.
- If you would like an appointment, ask your child’s primary care provider for a referral.
- If you have a referral, call 206-987-2016 or 844-935-3467 (toll-free).
- How to schedule.
If you have any questions, please contact us at 206-987-2016 or 844-935-3467 (toll-free).
-
Find a doctor
- Meet the Neurosciences team.
-
Locations
- Seattle Children’s hospital campus: 206-987-2016 or 844-935-3467 (toll-free)
- Bellevue Clinic and Surgery Center: 206-987-2016 or 844-935-3467 (toll-free)
- Everett: 425-783-6200
- Federal Way: 206-987-2016 or 844-935-3467 (toll-free)
- Olympia: 206-987-2016 or 844-935-3467 (toll-free)
- Tri-Cities: 206-987-2016 or 844-935-3467 (toll-free)
- Wenatchee: 206-987-2016 or 844-935-3467 (toll-free)
-
Refer a patient
- Urgent consultations (providers only): call 206-987-7777 or 877-985-4637 (toll free).
- If you are a provider, fax a New Appointment Request Form (NARF) (PDF) (DOC) to 206-985-3121 or 866-985-3121 (toll-free).
- Send the NARF, chart notes and any relevant documentation to 206-985-3121 or 866-985-3121 (toll-free).
- View our complete Neurosciences Center referral guidelines.
What is a Chiari malformation?
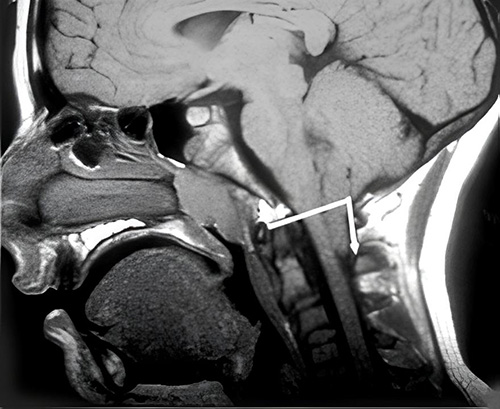 On this MRI image, the white line shows where the opening in the base of the skull (foramen magnum) is. The arrow shows the bottom parts of the cerebellum (cerebellar tonsils) pushing down into the top of the spinal canal. Photo courtesy of the Chiari and Syringomyelia Foundation.
On this MRI image, the white line shows where the opening in the base of the skull (foramen magnum) is. The arrow shows the bottom parts of the cerebellum (cerebellar tonsils) pushing down into the top of the spinal canal. Photo courtesy of the Chiari and Syringomyelia Foundation.In a Chiari malformation (key-AR-ee mal-for-MAY-shun), part of the brain (cerebellum) sits in the skull differently than normal. The reasons could be that the back of the skull is smaller or it has an unusual shape. Most often, this happens as the skull and brain form before birth. But it sometimes develops due to increased pressure on the brain from a condition like a tumor.
Some children with a Chiari malformation do not have symptoms. But the condition can cause headaches, balance problems or compression of the brain or spinal cord.
There are a few types of Chiari conditions.
- Chiari I malformation: Parts of the cerebellum (called the cerebellar tonsils) hang down through the opening in the base of the skull into the upper neck. This is the most common.
- Chiari II malformation: The bottom of the cerebellum (called the vermis) and parts of the brainstem hang down into the neck. Children with this type also have a form of spina bifida called myelomeningocele.
- Types III and IV are very rare.
- Secondary (acquired) Chiari malformations: Sometimes a condition that increases pressure on the brain causes a Chiari malformation. For example, a brain tumor or hydrocephalus can push the cerebellum down into the neck.
Having a child with a Chiari malformation usually does not increase the chance of having another child with this condition. Your doctor can talk with you about the chance for your family. A specific genetic change (mutation) has not been found in children with Chiari malformations.
Related conditions
Sometimes a child with a Chiari malformation has another condition that affects their brain, spinal cord or spine. These include:
- A cyst filled with cerebrospinal fluid (CSF) in the spinal cord. This is called syringomyelia or syrinx (ser-in-go-my-ILL-ee-uh). Some children with this condition also have a curved spine (scoliosis). If they do, treating the Chiari malformation and syrinx may stop the scoliosis from getting worse or even improve it.
- Spina bifida, a birth defect that leaves the spinal cord open and unprotected. All babies who have Chiari II malformations have spina bifida (PDF).
- A spinal cord that is pulled down and stuck in a child’s spinal canal (tethered spinal cord). This is a rare cause of Chiari I malformations.
Why choose Seattle Children’s for Chiari malformation treatment?
 Children from across the United States come to Seattle Children's for treatment of Chiari malformations. Our goal is to help your child get back to normal life, free of headaches or other symptoms. We will work with you to decide if surgery, other treatments or regular checkups are best for your child.
Children from across the United States come to Seattle Children's for treatment of Chiari malformations. Our goal is to help your child get back to normal life, free of headaches or other symptoms. We will work with you to decide if surgery, other treatments or regular checkups are best for your child.
- Your child will be in the hands of experts. Richard G. Ellenbogen serves on the scientific, education and advisory board of the nonprofit Chiari & Syringomyelia Foundation. He has treated more than 1,000 patients with Chiari malformation or syringomyelia.
- Seattle Children’s neurosurgery team is among the most experienced in the nation. We perform many more neurosurgeries than any other children’s hospital in our region. We also evaluate hundreds of children with Chiari malformations who do not need surgery. We do regular check-ins as they grow.
- In our Neurodevelopmental Clinic, experts in many medical areas work together to care for your child if a Chiari malformation causes problems in their thinking, balance, learning or emotions.
- We offer the most advanced diagnosis and treatments. For many children, MRI (magnetic resonance imaging) is part of making an accurate diagnosis. Our doctors have the equipment and expertise to use a special MRI (cine-MRI) that shows how CSF flows in and around the brain.
- Ellenbogen helped develop guidelines for using cine-MRI to diagnose Chiari malformations and for performing surgery for children with Chiari I and syringomyelia.
- For children who need urgent treatment, a reoperation or consultation, Seattle Children’s is the only hospital in the region with coverage 24 hours a day, 7 days a week by a pediatric neurosurgeon.
If you would like an appointment, ask your child’s primary care provider to refer you to our Neurosciences Center. If you have a referral, call 206-987-2016 to make an appointment. If you have questions, please contact us at 206-987-2016.
Providers, see how to refer a patient.
-
Research to advance care
- Ghayda Mirzaa is one of the few researchers in the world looking into how Chiari malformation happens. She studies brain tissue from children who have had surgery to learn how genes might affect the way the back of the brain develops. She also studies if genetic changes cause differences in Chiari malformation from one child to another.
- Ellenbogen does research on results of Chiari malformation surgery, with the goal of improving surgical techniques. He also uses MRI to better understand the flow of CSF around the brain and spinal cord.
- Children we treat have the option to take part in research studies of new treatments (clinical trials). They can be helpful if your child’s condition is not well controlled with standard medicines or surgeries.
Learn more about Seattle Children’s neurosciences research.
-
Specialists in caring for kids and teens
- Children don’t react to illness, injury, pain and medicine in the same way as adults. They need — and deserve — care designed just for them. Our team is specially trained to understand and meet your child’s needs.
- Our doctors are focused on how today’s treatment will affect your child as they develop and become an adult. Our experts base their treatment plans on years of experience and the newest research on what works best and is safest for your child.
-
Support for your whole family
- Learning that your child has a Chiari malformation can be stressful for the whole family. During visits, we take time to explain your child’s condition. We help you fully understand your treatment options so you can make choices that are best for your child.
- Our doctors, nurses, child life specialists and social workers help your child and your family through the challenges of their condition. We connect you to community resources and support groups.
- We work with families from the Northwest and beyond. Whether you live nearby or far away, we can help with financial counseling, schooling, housing, transportation, interpreter services and spiritual care. Read about our services for patients and families.
What are the symptoms of Chiari malformation?
Your child may not have symptoms. Symptoms are more likely if the malformation blocks the flow of CSF or puts pressure on the brain or spinal cord. Your child may have 1 or more of these:
- Headaches in the back of the head or headaches that get worse with straining, coughing or laughing
- Balance problems, which may cause trouble walking
- Neck pain
- Weakness
- Numbness
- Pain or tingling in their arms
- Quick eye movements they can't control, often from side to side
- Trouble with small motor tasks, such as writing or cutting with scissors
- Swallowing problems or reduced gag reflex
- Trouble breathing while asleep (sleep apnea)
Symptoms can happen at any time. They may start or get worse after an injury, physical effort or straining, such as exercising, coughing or sneezing.
-
Symptoms of more serious problems
Children with more extreme forms of Chiari malformation will have the same symptoms as for Chiari I malformation. But the symptoms are usually worse and advance more quickly.
Your child may have 1 or more of these:
- A high-pitched sound when breathing in (stridor), mainly when crying (Chiari II)
- Breathing tiny bits of food, fluid or saliva into the lungs (aspiration)
- Arm or leg weakness, numbness and tingling
How is Chiari malformation diagnosed?
Because a Chiari I malformation does not always cause symptoms, doctors may find it while they are checking your child for another reason. In babies with spina bifida, doctors do imaging studies shortly after birth and may find a Chiari malformation.
If doctors think your child might have a Chiari malformation, they will check your child’s:
- Balance
- Reflexes
- Motor skills
- Sense of touch
- Memory
- Thinking
Imaging studies
Doctors use imaging studies called MRI (magnetic resonance imaging) scans to look for Chiari malformations. These scans of the head and spine let doctors see if the bottom part of your child's cerebellum or brainstem is coming down into the space where the spinal cord enters the spine.
The scans can also help doctors know if pressure is being put on your child's cerebellum, brainstem or spinal cord. Often doctors order an MRI of the spine to check for syringomyelia, too.
Your child's doctors may use cine-MRI to see how CSF moves around the lower part of your child's brain. This is called a cine-MRI CSF flow study. Seattle Children’s has special computer software to make cine-MRI images. Our doctors are experienced in interpreting these images.
Cine-MRI helps doctors decide who may need surgery and which type would help most. Doctors also use it after surgery to tell how your child is doing.
Treating Chiari Malformations
Your child may not need treatment if their Chiari malformation does not cause symptoms or affect their daily life. If your child does need treatment, our goal is to help them get back to their life, without symptoms or limits on their usual activities. We offer medicines, physical therapy, occupational therapy and surgery options. Our neurosurgeons are skilled in procedures such as Chiari decompression to make extra space for the lower part of the brain and the spinal cord. Together, you and your child's doctor will decide whether your child needs treatment and which type is best.
-
Medicine and behavior changes
Medicine may help some symptoms. For example, pain medicines may help control headaches.
Your child's doctor may suggest avoiding certain activities, such as heavy lifting, that cause symptoms or make symptoms worse.
Physical and occupational therapy may help your child change how they do activities.
-
Deciding about surgery
To decide if surgery might help your child, we consider:
- What we find from your child's MRI
- Your child's symptoms and whether they can be managed with other treatment
- If your child has numbness, weakness, loss of balance, vision changes or other signs of problems with their brain, spinal cord or nerves
- If symptoms are getting worse
- Whether your child has syringomyelia
- Your family’s preference about whether to do surgery
Your child's doctor will talk with you in detail about the benefits and risks of surgery. Before surgery, your child may have imaging studies. These give the neurosurgeon more details about your child's skull and neck. Doctors use the information to plan the best way to do surgery for your child. Options include:
- X-ray
- CT (computed tomography) scan
- MRI (magnetic resonance imaging) scans
-
Surgery for Chiari malformation
The most common surgery for Chiari malformations is called posterior fossa decompression. The procedure:
- Makes more room in the skull for the cerebellum and brainstem. This relieves some pressure on the brain.
- Lets cerebrospinal fluid (CSF) flow in a more normal way, which may relieve some symptoms.
- In children with syringomyelia, lets the cyst drain, so your child doesn't need surgery on the cyst itself.
Your child's neurosurgeon will do most or all of these procedures:
- Remove bone from the base of the skull. This makes the normal hole in the base of the skull bigger so there's more room for the brain, spinal cord and CSF. Taking out the bone here is called suboccipital craniectomy.
- Remove the back part of the first bone of the spine (first cervical vertebrae or C1). This makes more room for your child's brain. This procedure is called C1 laminectomy. Some children who have surgery need only this procedure and suboccipital craniectomy.
- Open the membrane that covers your child's brain, where the bone was removed from the skull. This makes more room for CSF to flow. Most children need this step.
- Shrink the bottom parts of the cerebellum, using a tool that is heated by an electric current (electrocautery). This makes more room for CSF flow.
- Patch the membrane. The surgeon uses tissue from under your child's scalp to create a natural patch and give the brain and CSF more room.
- Close the incision by bringing the skin back together.
-
After surgery
After surgery, we will give your child medicine to help ease pain and relax their muscles while they heal. Often children do not remember much about this healing time. Most children stay in the hospital 1 to 3 days after surgery.
If needed, we will give your child corticosteroids to reduce any swelling or reaction to the operation.
Follow-up care is important after surgery to watch for any symptoms that come back or get worse. In most children, symptoms of a Chiari malformation start to improve during the first weeks after surgery. Some children continue to have symptoms.
For the first few months while they heal, and perhaps longer, it is important that your child does not strain their neck too much. Your care team will let you know which activities your child should avoid, like heavy lifting and contact sports.
The goal of the operation is to return your child to school, sports and full activities.
Read our handout Chiari Decompression: Care After Surgery (PDF) (Spanish)
-
Treatment and follow-up for related conditions
Sometimes children with Chiari malformation will need treatment for another condition that affects their brain, spinal cord or spine, such as:
- Syringomyelia, a cyst filled with CSF in the spinal cord
- Myelomeningocele or other neural tube defects
- A curved spine (scoliosis)
Children with these conditions will need regular check-ups throughout life. Your doctor will look for new symptoms and check that any existing symptoms are not getting worse. Your child may benefit from these Seattle Children’s experts:
- Our Neurodevelopmental team cares for children who have problems with learning, emotions or behavior. Doctors, nurses, social workers, dietitians, physical therapists and occupational therapists work together to meet your child's needs. We also help you find resources in your community.
- Our Spine Program is known nationally for treating all kinds of spine problems in children.
Contact Us
If you would like an appointment, ask your child’s primary care provider for a referral. If you have a referral, call 206-987-2016.
Providers, see how to refer a patient.
If you have questions, contact us at 206-987-2016.
Paying for Care
Learn about paying for care at Seattle Children’s, including insurance coverage, billing and financial assistance.
For Healthcare Professionals
-
Schedule an appointment with the Neurosciences Center
If this is a medical emergency, call 911.
- If you would like an appointment, ask your child’s primary care provider for a referral.
- If you have a referral, call 206-987-2016 or 844-935-3467 (toll-free).
- How to schedule.
If you have any questions, please contact us at 206-987-2016 or 844-935-3467 (toll-free).
-
Find a doctor
- Meet the Neurosciences team.
-
Locations
- Seattle Children’s hospital campus: 206-987-2016 or 844-935-3467 (toll-free)
- Bellevue Clinic and Surgery Center: 206-987-2016 or 844-935-3467 (toll-free)
- Everett: 425-783-6200
- Federal Way: 206-987-2016 or 844-935-3467 (toll-free)
- Olympia: 206-987-2016 or 844-935-3467 (toll-free)
- Tri-Cities: 206-987-2016 or 844-935-3467 (toll-free)
- Wenatchee: 206-987-2016 or 844-935-3467 (toll-free)
-
Refer a patient
- Urgent consultations (providers only): call 206-987-7777 or 877-985-4637 (toll free).
- If you are a provider, fax a New Appointment Request Form (NARF) (PDF) (DOC) to 206-985-3121 or 866-985-3121 (toll-free).
- Send the NARF, chart notes and any relevant documentation to 206-985-3121 or 866-985-3121 (toll-free).
- View our complete Neurosciences Center referral guidelines.