Velopharyngeal Dysfunction
-
Schedule an appointment with the Childhood Communication Center
- If you would like an appointment, ask your child’s primary care provider for a referral.
- If you have a referral, call 206-987-3853.
- How to schedule.
If this is a medical emergency, call 911.
-
Find a doctor
- Meet the Childhood Communication Center team.
-
Locations
- Seattle Children’s hospital campus: 206-987-3853
-
Refer a patient
- Urgent consultations (providers only): call 206-987-7777 or, toll-free, 877-985-4637.
- If you are a provider, fax a New Appointment Request Form (NARF) (PDF) (DOC) to 206-985-3121 or 866-985-3121 (toll-free).
- No pre-referral work-up is required for most conditions. If you have already done a work-up, please fax this information as well as relevant clinic notes and the NARF to 206-985-3121 or 866-985-3121 (toll-free).
- View our complete Childhood Communication Center referral information.
What is velopharyngeal dysfunction?
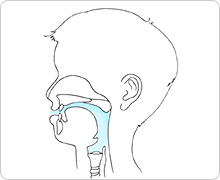 Typical speech: A closed soft palate pushes airflow (shown in blue) through the mouth.
Typical speech: A closed soft palate pushes airflow (shown in blue) through the mouth.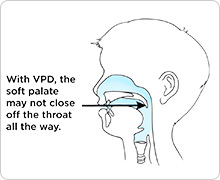 Speech with VPD: An open soft palate lets air flow through the nose and mouth (shown in blue).
Speech with VPD: An open soft palate lets air flow through the nose and mouth (shown in blue).
In velopharyngeal dysfunction (VPD), parts of the throat and roof of the mouth do not work right during speech.
The condition is pronounced vee-lo-fare-in-GEE-al dis-FUNK-shun.
- “Velo” refers to the velum, or soft palate. It is the part of the roof of the mouth that moves when you say “ah.”
- “Pharyngeal” refers to the throat (pharynx).
For many sounds during normal speech, the palate rises to touch the back of the throat and sends all of the air out of the mouth.
When a child has VPD, their soft palate does not always contact their throat when they talk. This lets air escape through their nose during speech.
If VPD is severe, it may be hard to understand your child’s speech.
What are the different types of VPD?
Determining the specific type of VPD your child has is very important so we can recommend the right treatment. There are 3 types.
-
Velopharyngeal insufficiency (VPI)
Velopharyngeal insufficiency (VPI) occurs when there is not enough (“insufficient”) tissue in the palate or throat to let the palate contact the back of the throat during speech.
-
Velopharyngeal mislearning (VPM)
Velopharyngeal mislearning (VPM) happens when a child learns wrong ways to make sounds. Some children develop unusual speech patterns that do not use the palate even though their palate works properly.
Other children use unusual speech patterns to make up for problems with the structure of their mouth or throat. They learn to make sounds without moving their soft palate to the back of their throat.
-
Velopharyngeal incompetence (VP incompetence)
Velopharyngeal incompetence (VP incompetence) means there is a problem in how the soft palate moves to make speech sounds.
It is possible to have more than one type of VPD. A speech and language pathologist (SLP) specializing in VPD will help determine what types your child has.
Velopharyngeal Dysfunction at Seattle Children’s
Most families have not heard of velopharyngeal dysfunction before their child is diagnosed with it. Seattle Children’s has a great deal of experience treating VPD. Our Childhood Communication Center has a clinic focused on VPD. Each year our Craniofacial Center cares for more than 1,000 children with cleft palate, which increases the chance of having VPD.
-
Specialties to cover your child’s needs
Your child’s treatment team is likely to include:
- A speech and language pathologist (SLP) who specializes in identifying traits of VPD speech. SLPs also are skilled at telling VPD apart from other speech problems.
- An ear, nose and throat doctor (ENT or otolaryngologist). Our experienced ENTs do special tests to check velopharyngeal function in children and perform surgery if needed.
- A surgeon skilled in doing surgeries on the throat and palate to help correct speech issues. Depending on your child’s needs, this may be an ENT surgeon or a plastic surgeon.
- An orthodontist who makes custom speech appliances for children who need them.
If your child’s VPD is related to a craniofacial condition, they will also receive care from other experts in our Craniofacial Center. These 50 specialists work together to diagnose and create a personalized plan of care for each child. A craniofacial pediatrician, nurse and social worker will work closely with your family. They help coordinate care and make sure all your questions are answered.
-
Guidance to prevent speech problems
An SLP starts working with you and your baby during their first year of life. Even before they learn to talk, babies are making pre-speech sounds.
Babies with cleft palate often are finding ways to make sounds that do not require their palate to touch the back of their throat.
Our speech and language pathologists monitor your child closely for development of VP mislearning. We can help you encourage your child to develop correct speech patterns even before their palate is repaired.
-
Support for your whole family
Families may face many challenges when their child has VPD. Often, a child already has been treated for cleft palate or other medical conditions. It can be hard to choose among the possible treatments.
We take time to explain your child’s condition and answer all your questions. We help you fully understand your treatment options and make choices that are right for your family.
Our SLPs and social workers help you deal with the challenges and find resources in your community.
Symptoms of Velopharyngeal Dysfunction
Symptoms vary depending on the type of VPD your child has.
-
Velopharyngeal insufficiency symptoms
The 2 main speech symptoms of VPI are:
- Nasal speech (hypernasality)
- Nasal air escape
Both symptoms happen because the palate does not touch the back of the throat during speech.
Nasal speech
In English, the sounds m, n and ng are the only sounds that should sound nasal. Nasal speech happens when other sounds resonate through the nose. This is called “hypernasality” or “hypernasal resonance.” It can be mild or severe.
You can hear nasal speech when a child is saying vowels or sounds such as w, y, l or r.
Nasal air escape
When air escapes through the nose as your child makes pressure consonants, this is called “nasal air escape” or “nasal air emission.”
In English, the pressure consonants are p, b, t, d, k, g, s, z, f, v, sh, zh, ch, dj and th.
They are called pressure consonants because pressure builds up in the mouth when the palate closes and seals off the mouth from the nose.
When a child has VPI, pressure cannot build up in the mouth. Air escaping through the nose can sound like puffs, squeaks or snorts. Your child’s speech may be very soft.
To learn more, see Early Sound Development in Children with a Cleft Palate (PDF) (Spanish).
-
Velopharyngeal mislearning symptoms
Sometimes children learn the wrong way to make sounds. During speech their soft palate does not close to the back of their throat. These sounds are called “compensatory misarticulations.” They include:
- Stopping air with the vocal cords (as when saying “uh oh”). This sound is called a glottal stop.
- Using the tongue or palate to stop or restrict air in the mouth or throat in unusual ways.
- Holding the palate open and pushing air through the nose
-
Velopharyngeal incompetence symptoms
Symptoms of VP incompetence vary widely. They are caused by a problem with how the soft palate moves to make speech sounds. The timing of palate movement or the amount the palate moves may be wrong.
Diagnosising Velopharyngeal Dysfunction
Before we develop a treatment plan, we determine what type of VPD your child has. We also check for other issues that affect speech.
Your child may have trouble with:
- Making sounds with the mouth and tongue (articulation)
- Putting the sounds together (speech coordination)
- Weak speech muscles
- Speech sounding “stuffed up” (hyponasality)
- Using their vocal cords to make sounds
- Hearing
Your child may need 1, 2 or 3 appointments to complete an evaluation for VPD. Before someone calls to schedule, an SLP specializing in VPD will determine which appointments your child may need. After the tests, we will talk to you about treatment options. Learn more about what to expect at a VPD Clinic visit.
For more information, see:
- Evaluating VPD in Your Child (PDF) (Spanish)
Treating VPD
Our goal is to eliminate VPD as early as possible. This helps your child develop normal speech patterns.
At your first appointment, we determine which kind of VPD your child has. The 3 types of VPD have different treatments:
- VPI is treated with surgery or a special speech appliance that your child wears in their mouth.
- VPM is treated with speech therapy.
- VP incompetence is treated with speech therapy and sometimes with a speech appliance or surgery.
-
Speech therapy
Speech therapy may be part of your child’s treatment even if they have a structural problem that will also require surgery or a speech appliance.
- For children with VPM, speech therapy can help them learn how to control air flow and use their tongue, lips and jaw correctly to make sounds.
- With VP incompetence, the specific goals of speech therapy depend on your child’s needs. After assessing your child, the SLP will determine which sounds and skills to focus on.
-
Speech appliance

For some children with VPI or VP incompetence, treatment will include a speech appliance called an obturator.
An obturator is like a modified dental retainer with a “speech bulb” attached to the back. It can help your child sound less nasal and keep air from escaping out of their nose when they talk.
The obturator is custom shaped to fit your child’s muscle movements. Your child will have several visits to the Dental Clinic so the dentist can make the appliance.
A speech and language pathologist helps fit the obturator and check how effective it is. Your child wears it during the day and takes it out at night for sleep. It can be worn while eating.
An obturator can be a short- or long-term option. It can be used before or instead of surgery for VPI. Some children start with an obturator and have surgery when they are older. Some continue to use an obturator as adults
-
Speech surgery
Most children with VPI need surgery because they don’t have enough (“insufficient”) tissue in the palate or throat. Sometimes children with VP incompetence also need surgery.
If your child could benefit from surgery, your surgeon and SLP will talk with you about the type of surgery and when to have it.
The most common speech surgeries for VPI are called Furlow palatoplasty and sphincter pharyngoplasty.
The Furlow palatoplasty brings the muscles of the palate into a more normal position. This lengthens the palate.
Sphincter pharyngoplasty moves tissue from the side of the throat to create a “speed bump” at the back of the throat. With this change, the soft palate can touch the back of the throat when your child talks.
After VPI surgery, the soft palate can touch the back of the throat to close off the nose during speech.
Surgical procedures are performed inside the mouth under general anesthesia. Most times, your child will need to stay in the hospital overnight.
Your child will have a follow-up speech evaluation 3 to 4 months after surgery.
Contact Us
Our VPD Clinic is part of the Childhood Communication Center. Call 206-987-3853 for an appointment or more information.
For questions about cleft palate care, contact the Craniofacial Center at 206-987-2208.
-
Schedule an appointment with the Childhood Communication Center
- If you would like an appointment, ask your child’s primary care provider for a referral.
- If you have a referral, call 206-987-3853.
- How to schedule.
If this is a medical emergency, call 911.
-
Find a doctor
- Meet the Childhood Communication Center team.
-
Locations
- Seattle Children’s hospital campus: 206-987-3853
-
Refer a patient
- Urgent consultations (providers only): call 206-987-7777 or, toll-free, 877-985-4637.
- If you are a provider, fax a New Appointment Request Form (NARF) (PDF) (DOC) to 206-985-3121 or 866-985-3121 (toll-free).
- No pre-referral work-up is required for most conditions. If you have already done a work-up, please fax this information as well as relevant clinic notes and the NARF to 206-985-3121 or 866-985-3121 (toll-free).
- View our complete Childhood Communication Center referral information.