Nimble, Flexible, Responsive
Seattle Children’s collaborates with peers close to home and across the U.S. to solve puzzles presented by COVID-19
Published in Connection magazine, Spring 2020
The emergence and rapid spread of SARS-CoV-2, the novel virus that can cause COVID-19, presents the global community with a variety of challenges on an unprecedented scale.
As news of the virus began to emerge, Seattle Children’s researchers, clinicians and staff quickly began pivoting their efforts to better understand and respond to the developing pandemic.
“We’re examining the virus from all angles so we can understand why COVID-19 affects children differently than other populations, and to address the burden it presents to children and families,” says Dr. Leslie Walker-Harding, Seattle Children’s chief academic officer. “What we learn will help reduce the overall impact of the pandemic and help us prepare for a potential repeat outbreak of this or another novel respiratory virus that targets children and other vulnerable populations.”
Seattle Children’s has more than 50 COVID-19 related research studies underway seeking to understand how this virus is transmitted in children, why it affects children differently than adults, how it functions in the body, and ways we can treat and prevent it.
Here are just a few examples of the research and innovations that began this spring in response to COVID-19. New efforts continue as this rapidly evolving situation unfolds.
Is it different for kids?

Seattle Children's already has more than 50 COVID-19 related research studies underway, including one co-led by Dr. Whitney Harrington (above), to better understand how the virus affects children.
“I’m really impressed by how quickly many members of our center shifted to focus on COVID-19 related projects and the level of collaboration with other local institutions,” says Dr. Whitney Harrington, an infectious disease specialist and investigator in Seattle Children’s Center for Global Infectious Disease Research (CGIDR).
Harrington is teaming with CGIDR’s co-director, Dr. Lisa Frenkel, on a study that will track 1,000 healthy Seattle Children’s employees and their immediate family members for one year to understand if factors in their blood or nasal secretions can predict whether they will have symptoms if they later get infected with SARS-CoV-2. This knowledge could provide insights into treatment for individuals with severe COVID-19.
The study will contribute valuable epidemiological data from a community cohort on who is becoming infected, when they’re becoming infected, and who is getting sick from the infection. The researchers also hope to compare the immune responses of study participants who develop no or mild symptoms to those who develop COVID-19 using a systems biology approach.
“It’s unclear whether children are less susceptible to infection or whether they acquire infection at the same rate as adults but aren’t getting sick,” says Harrington. “That’s one of the key questions we want to understand in our study.”
Testing the 1st vaccine
The Coler Lab (led by Dr. Rhea Coler, a senior investigator in CGIDR) is supporting the world’s first-in-human clinical trial of an experimental coronavirus vaccine. Funded by the National Institute of Allergy and Infectious Diseases (NIAID), the study is being conducted at Kaiser Permanente Washington Health Research Institute in Seattle, which is part of NIAID’s Infectious Diseases Clinical Research Consortium.
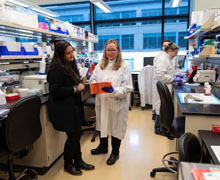
Collaboration is the key to combating emerging global health threats says Dr. Rhea Coler (at left with senior research scientist Dr. Susan Baldwin). The Coler Lab is supporting the world's first clinical trial in people of a vaccine for SARS-CoV-2.
Coler’s team is isolating cells and plasma from the blood samples of study participants who received the experimental vaccine. Investigators at the Vaccine Research Center at the National Institutes of Health (NIH) then analyze the samples to determine whether various doses of the vaccine induce the types of responses that may offer protection against SARS-CoV-2.
“Our collaborators at Kaiser immunized the first individual in mid-March – just over 60 days after the virus was first sequenced,” says Coler. “I am pleased to play a small but not insignificant role in the overall vaccine research and development efforts to tackle this rapidly spreading viral disease. The pandemic response is a fantastic example of how much we can accomplish when we work rapidly and efficiently together, and how essential public-private collaborative coordination is in combating emerging global health threats such as those caused by SARS-CoV-2."
Solving structural secrets
Another collaborative research effort led by Dr. Peter Myler has already contributed findings about SARS-CoV-2 for vaccine development efforts, and new knowledge generated daily is expected to aid in drug development.
Myler, a principal investigator at Seattle Children’s, also serves as director of the Seattle Structural Genomics Center for Infectious Disease* (SSGCID), an NIAID-funded consortium that includes teams from Seattle Children’s Research Institute, UCB, the University of Washington, and Washington State University.
The consortium works to solve the 3D structure of proteins from infectious disease organisms and give insights into their function. That information can be used to develop vaccines, new drugs and even diagnostics for clinical use. To date, SSGCID has solved more than 1,250 protein structures, including two from SARS-CoV-2.
“Within two months of having the sequencing information, our cryoEM lab, headed by David Veesler at the University of Washington, solved the structure of the major viral surface protein,” Myler says.
“Some might ask ‘why do this type of basic research?’ I mean, who cares what a protein looks like? Well, one reason is so that we’re ready when a threat like COVID-19 emerges, and we can move very quickly to get the answers needed to make an impact against the disease.”
Telehealth takes off

Maile Harvard, RN, and other Seattle Children's providers began using telemedicine within the hospital to limit the number of providers at a patient's bedside. This innovation protects patients and healthcare workers from exposure and minimizes the use of personal protective equipment.
Seattle Children’s quickly stepped up use of telehealth technologies so we could provide another way for our patients to access care during the pandemic – within the hospital and throughout our region.
“Typically, when you think about telemedicine, there are miles of physical distance between the patient and the healthcare team,” says Dr. Joan Roberts, a member of Seattle Children’s Critical Care team. “We’re using telemedicine where the provider is right outside the patient’s room. It helps protect patients and healthcare workers from exposure and minimizes the use of personal protective equipment.”
By mid-March, Seattle Children’s had 20 telehealth devices within the hospital deployed in areas like the Emergency Department, Intensive Care Unit, Cancer and Blood Disorders Center, and the special 20-bed isolation unit for patients with potential or confirmed cases of COVID-19.
Applying telemedicine in this way lends eyes and ears in a patient’s room while reducing the number of healthcare workers needed at the bedside. The technology has changed the way Seattle Children’s responds to complex emergency resuscitations known as Code Blue. Instead of having the entire Code Team in the room, a camera in the patient’s room is hooked up to a monitor outside the room where the Code Team leader runs the code. More than half of the team is also outside the room getting everything ready, supporting the few people inside the room.
The pandemic also catapulted Seattle Children's utilization of telehealth visits. We piloted home telehealth visits two years ago with a select number of patients, a few specialties, and plans to scale slowly. That plan changed in March 2020, and by April, clinics across the system were using telehealth visits with at-home videoconferencing in earnest.
“In times of crisis, innovation gets us through,” says Hue Chiang, manager, Innovation & Design. “My hope is that even after the COVID-19 pandemic we continue to use our collective brain power to approach big problems by thinking differently.”